|
 |
- Search
AbstractObjectivesBenign paroxysmal positional vertigo (BPPV) can be treated using a simple repositioning maneuver. This study demonstrates the effects of early repositioning therapy in patients with BPPV, especially with regard to recurrence.
MethodsWe enrolled 138 consecutive patients who had been diagnosed with BPPV in the emergency rooms and ENT out-patient clinics of Chung-Ang University Hospital and Samyook Medical Center from January to June 2009. All patients immediately underwent appropriate canalith repositioning procedures (CRPs) depending on canalith type and location. The CRPs were performed daily until the patient's symptoms were resolved. The patients were classified into two groups according to the duration between symptom onset and initial treatment: less than 24 hours (early repositioning group, n=66) and greater 24 hours (delayed repositioning group, n=72). We prospectively compared the numbers of treatments received and the recurrence rates between the two groups.
ResultsFollow-up periods ranged from 8 to 14 months, 77 cases involved posterior canal BPPV, 48 cases were lateral canal BPPV (of which 20 cases were cupulolithiasis), and 13 cases were multiple canal BPPV. BPPV recurrence was found in a total of 46 patients (33.3%). The necessary numbers of CRPs were 2.3 for the early repositioning group and 2.5 for the late repositioning group, a difference that was not statistically significant (P=0.582). The early repositioning group showed a recurrence rate of 19.7%, and the delayed repositioning group showed a recurrence rate of 45.8% (P=0.002).
Benign paroxysmal positional vertigo (BPPV) is the most common cause of dizziness, responsible for about 20% of cases (1, 2). Diagnosis is simple compared to those of other dizziness-related diseases since specific nystagmus due to excitement of the semicircular canal can be revealed by a careful history combined with Frenzel glass or video imaging.
When the otolith is displaced from the utricule to the rotational movement-detecting semicircular canal, severe dizziness is experienced due to the reaction of the semicircular canal. The displacement of the otolith to the semicircular canal is the most convincing theory to explain nystagmus and the associated symptoms, serving as the basic concept for canalith repositioning procedures (CRPs). There are many types of CRPs, categorized by the affected semicircular canal and the type of otolith. Regardless of affected canal, BPPV is shown to have a high treatment rate by CRPs (3, 4).
Even though BPPV may be easily treated with CRPs, BPPV patients who visit a non-ENT clinic or emergency room often experience sustained symptoms and are treated with only medication (vestibular suppressants, antiemetics) because non-ENT doctors are often unaware of BPPV and CRP treatment options. In these cases, accurate diagnosis is delayed and treatment may be difficult.
Although CRP is a relatively successful treatment for BPPV, recurrence is high, with a reported one-year recurrence rate of 22.6-30% (5-7). So, recurrence can be an important prognostic factor. Many factors may lead to recurrence, but to date there has been no study of the relationship between the time between symptom onset and CRP with recurrence.
The purpose of this study is to demonstrate the effects of early repositioning therapy in patients with BPPV, especially with regard to recurrence.
This study included 138 patients diagnosed with BPPV in the emergency rooms and ENT out-patient clinics in Chung-Ang University Hospital and Samyook Medical Center between January-June 2009. The last follow-up visit took place in February 2010, and follow-up durations ranged from 8 to 14 months. The study is prospective, using histories and the results of vestibular function tests. By taking careful histories, we were able to investigate the past history of vertigo, upper respiratory infection symptoms, otitis media, hypertension, tuberculosis, anemia, menstruation, occupation (to determine exposure to noise, agricultural pesticides, use of vibrating machinery, etc.), medications (antihypertensives, anticonvulsants, muscle relaxants), and trauma. Patients who had been treated for similar vertigo experiences or who had been treated with medication prior to repositioning therapy were excluded. We diagnosed BPPV in patients showing true vertigo by positional changes, rotating nystagmus on a Frenzel glass or video image, three consecutive nystagmuses, normal eye movement, no signs of spontaneous nystagmus, and normal neurological examinations including a fixation test and tandem gait and neurological exams (cerebellar function test, 12 cranial nerve test, and upper and lower limb motor/sensory nerve test).
All treatments were performed by a skilled ENT doctor. For CRP of posterior canal BPPV, we applied a modified Epley's maneuver, while a Barbecue maneuver was used for lateral canal BPPV. CRP was performed immediately after diagnosis, and we recorded the time between symptom onset and initial CRP. CRP was then performed daily until typical positional nystagmus disappeared. The patient was considered to be cured when whirling dizziness disappeared on a positional test and when positional nystagmus disappeared on a video nystagmus test. We instructed the patients to immediately return to the hospital if BPPV symptom recurred. The follow-up periods ranged from 8-14 months, and patients who did not return voluntarily were called at approximately 2-3 month intervals to check for BPPV symptom. We defined recurrence as the reappearance of a similar whirling dizziness or reappearance of a similar rotating nystagmus.
For emergency room patients, the time between symptom onset and initial treatment was generally a few hours, while that for clinic patients was generally greater than one day. Patients were thus classified into two groups: the early repositioning group (less than 24 hours to first treatment) and the delayed repositioning group (greater than 24 hours to first treatment) (Table 1). The required numbers of CRPs and the recurrence rates were compared between the two groups. Statistical analysis was conducted using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA), and cutoff points were determined according to logistic regression analysis. Pearson's chi-square test, Fisher's exact test and an independent t-test were used for analysis, and P-values less than 0.05 were considered statistically significant.
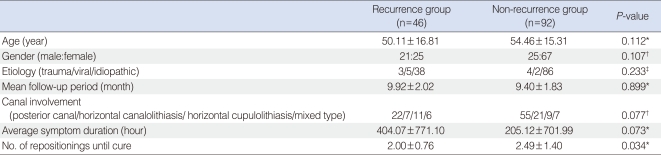
Age, gender, causative factors, and frequency of the affected semicircular canal were included in the analysis. The mean age was 51.56┬▒16.39 years (range, 9 to 80 years), 46 patients were males, 92 were females and most causative factors were idiopathic. Categorizing according to semicircular canal showed that 77 patients were affected in the posterior canal, 48 were affected in the lateral canal and 13 were affected in multiple canals. There were no significant differences in age, gender, causative factors or affected semicircular canal between the two groups (Table 2).
The overall recurrence rate was 33.3% (46 out of 138 subjects), and the average required number of treatments was 2.4 times. The number of treatments and the recurrence rates were analyzed by age, gender, causative factors, affected semicircular canal, canalolithiasis or cupulolithiasis type, and no significant differences were observed (data not shown). In the logistic regression analysis, considering only the sensitivity resulted in a cutoff point at hour 6. However, considering both sensitivity and specificity as well as the pre-determined result which showed that the number of treatments received, the cutoff point was set at 24 hours after symptom onset (Table 1). The average numbers of treatments received before full recovery was 2.5 in the early repositioning group and 2.3 in the delayed repositioning group, and the difference was not statistically significant (P=0.582). The recurrence rate was 19.7% in the early repositioning group and 45.8% in the delayed repositioning group, a significant difference (P=0.002) (Table 2).
Classifying the patients according to recurrence, we found that more males suffered from recurrence, although the gender difference was not statistically significant (Table 3). No other factors were found to be significant.
Benign paroxysmal positional vertigo is a common disease with a life-time prevalence of 2.4% (8). Patients with the disease often visit the emergency room due to sudden dizziness. However, such patients are often not correctly diagnosed or treated, just receiving a fluid injection and antiemetics before being discharged with vestibular suppressants and drugs to improve blood circulation.
Many opinions regarding BPPV treatment have existed. Since the spontaneous recovery rate is high and most of the patients are older, some specialists support simple observation, whereas others choose medication therapy because it is economical, convenient and yields rapid results (9). But, repositioning therapy has a remarkably higher alleviation rate and a shorter recovery time. Therefore, it is possible to prevent habitualization and fear of dizziness since the return to normal life is rapid and the symptom duration is short. As a result, repositioning therapy is widely used as the primary BPPV treatment (7, 10, 11), and its effectiveness has been shown through conventional studies (7), meta analyses (12), case-control studies (10, 13), and cohort studies (14). There have been reports that BPPV patients who received repositioning therapy in the emergency room or family medicine clinic showed more improvement compared to that of a control group. It has also been reported that decreased symptom duration has lead to improved quality of daily life for affected individuals (15).
In this study, we analyzed the relationship between the time of initial CRP treatment, the number of CRP treatments, and prognosis.
Initailly we hypothesized that early treatment may reduce the number of treatments necessary for complete remission based on below explanations. First, when repositioning therapy is delayed, the probability of cupulolithiasis increases, leading to difficulties in otolith displacement using only a simple positional maneuver. Also, the time required for stabilization after repositioning therapy is extended, and longer periods of clinical stabilization are difficult to achive (16). Second, as treatment is delayed, the duration of dizziness is increased, and the central nervous system needs more time to readapt after repositioning therapy. Additionally, the extended dizziness results in escalated patient fear and low compliance, which reduces overall treatment efficacy. But, in our study, The correlation between the time between symptom onset and initial treatment and the number of treatments required was not statistically significant (P=0.582) (Table 2).
Our repositioning therapy and assessment were conducted one day interval for the following two reasons. First, since BPPV is due to the displacement of the otolith, symptoms are instantly cured upon repositioning. Second, we wanted to exclude biases due to the high spontaneous recovery rate, 30% in the first week and 64% in the first month (17). There are many different variations in the frequency of repositioning treatments (it may be performed only once (18), performed a fixed number times per visit or performed repeatedly until dizziness or nystagmus disappears (19). However, no differences between these variations have been found on short-term follow-up.
The recurrence rate for the early repositioning group was significantly lower than that of the delayed repositioning group (P=0.002) (Table 2). We offer possible explanations for this result. In the early repositioning group, the otolith is rapidly relocated into the utricle and causes no anatomical deformities. In delayed repositioning, however, the otolith is aggregated and forms a heavier mass, often leading to recurrence. If the otolith remains in the semicircular canal for a period of time, it may partially obstruct the canal or prevent endolymphatic fluid absorption, the presumed the reason for endolymphatic hydrops, an anatomical deformity of the labyrinth. Also, repetitive hydrops leads to circulation difficulties in the macula and irreversible damage on the macular surface, and the resulting otoconia repeatedly enter the semicircular canal, increasing the rate of recurrence (20). Also, as treatment is delayed, continuous stimulation of the otolith leads to higher recurrence due to degenerative changes in the labyrinth.
Dorigueto et al. (5) found a recurrence rate of 26% in 100 BPPV patients one year after treatment. Del Rio et al. (6) reported a recurrence rate of 22.6% in 104 patients over a 6-15 month follow-up. Nunez et al. (7) calculated the yearly recurrence rate after repositioning therapy to be 15%. Blakely (21) showed 30% recurrence in patients, of which 10% were in the first year and the remaining 20% were between 18-36 months. Compared to these reports, our recurrence rate was high, 33.3% over 8-14 months. This may be simply due to more actual recurrence or to the fact that we more rigorously investigated recurrence.
In literature, the prognostic factors for repositioning therapy are age, gender, causative factors, pathogenesis, affected semicircular canal, mastoid vibrator use, treatment method, treatment skill and treatment interval (22). In our study, age, gender and affected semicircular canal showed no statistical correlation with the number of treatments or with recurrence rate, similar to the results of Nunez et al. (7) (Table 3). Our study was idiopathic in many cases, and the use of mastoid vibrators was not analyzed due to lack of data.
In conclusions, BPPV is one of the most common diseases involving dizziness. Even though repositioning therapy is effective, further work is needed to address its high recurrence rate. The early performance of repositioning therapy has been shown to decrease recurrence and allow for early recovery due to the rapid relief of symptoms. Also, it may be necessary for non-ENT primary doctors to familiarize themselves with concept of BPPV and repositioning therapy so that early diagnosis and adequate consultation or treatment are achieved.
References1. Kroenke K, Hoffman RM, Einstadter D. How common are various causes of dizziness? A critical review. South Med J. 2000 2;93(2):160-167. PMID: 10701780.
2. Nedzelski JM, Barber HO, McIlmoyl L. Diagnoses in a dizziness unit. J Otolaryngol. 1986 4;15(2):101-104. PMID: 3712537.
3. Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope. 1999 4;109(4):584-590. PMID: 10201745.
4. Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992 9;107(3):399-404. PMID: 1408225.
5. Dorigueto RS, Mazzetti KR, Gabilan YP, Gananca FF. Benign paroxysmal positional vertigo recurrence and persistence. Braz J Otorhinolaryngol. 2009;Jul-Aug;75(4):565-572. PMID: 19784427.
6. Del Rio M, Arriaga MA. Benign positional vertigo: prognostic factors. Otolaryngol Head Neck Surg. 2004 4;130(4):426-429. PMID: 15100638.
7. Nunez RA, Cass SP, Furman JM. Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2000 5;122(5):647-652. PMID: 10793340.
8. von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007 7;78(7):710-715. PMID: 17135456.
10. Hilton M, Pinder D. The Epley manoeuvre for benign paroxysmal positional vertigo: a systematic review. Clin Otolaryngol Allied Sci. 2002 12;27(6):440-445. PMID: 12472509.
11. Smouha EE. Time course of recovery after Epley maneuvers for benign paroxysmal positional vertigo. Laryngoscope. 1997 2;107(2):187-191. PMID: 9023241.
12. Lopez-Escamez JA, Lopez-Nevot A, Salinero J. The treatment of benign paroxysmal positional vertigo of the lateral semicircular canal by positional manipulation. Acta Otorrinolaringol Esp. 1999;Aug-Sep;50(6):473-475. PMID: 10502701.
13. Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 1998 7;118(4):455-460. PMID: 9726666.
14. Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987 3;37(3):371-378. PMID: 3822129.
15. Kang BS, Choi PJ, Im TH, Bae SM, Song HG, Song GJ, et al. Efficacy of otolith repositioning maneuver and its clinical features in benign paroxysmal positional vertigo. J Korean Soc Emerg Med. 2002 9;13(3):256-261.
16. Jo SW, Chung WK, Park JH, Bae JH, Han DH, Lee WS. Effectiveness of cupulolith repositioning maneuver in the treatment of lateral semicircular canal cupulolithiasis. Korean J Otolaryngol-Head Neck Surg. 2000 11;43(11):1147-1157.
17. Seo T, Miyamoto A, Saka N, Shimano K, Sakagami M. Immediate efficacy of the canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo. Otol Neurotol. 2007 10;28(7):917-919.
18. O'Reilly RC, Elford B, Slater R. Effectiveness of the particle repositioning maneuver in subtypes of benign paroxysmal positional vertigo. Laryngoscope. 2000 8;110(8):1385-1388. PMID: 10942146.
19. Gross EM, Ress BD, Viirre ES, Nelson JR, Harris JP. Intractable benign paroxysmal positional vertigo in patients with Meniere's disease. Laryngoscope. 2000 4;110(4):655-659. PMID: 10764014.
20. Rhee CK. Benign Paroxysmal positional vertigo. Korean J Otolaryngol-Head Neck Surg. 2004 6;47(6):491-506.
21. Blakley BW. A randomized, controlled assessment of the canalith repositioning maneuver. Otolaryngol Head Neck Surg. 1994 4;110(4):391-396. PMID: 7848400.
22. Macias JD, Lambert KM, Massingale S, Ellensohn A, Fritz JA. Variables affecting treatment in benign paroxysmal positional vertigo. Laryngoscope. 2000 11;110(11):1921-1924. PMID: 11081611.
|
|
|||||||||||||||||||||||||||||||||||||||||