INTRODUCTION
Hamartomas are non-neoplastic malformations or inborn errors of tissue development first described in 1904. Hamartomas can occur in any area of the body, but commonly originate from the spleen, intestine, and lung [1]. However, hamartomas in the upper aerodigestive tract are very rare [2]. In 1995, Birt and Knight-Jones [3] reported the fisrt case of a harmatoma in the upper aerodigestive tract. In 1995, Wenig and Heffner [4] documented the clinicopathologic features of 31 cases of hamartoma and introduced the term respiratory epithelial adenomatoid hamartoma (REAH) as one particular type of hamartoma. Approximately 70% of REAHs occur in the nasal cavity, most often localized to the posterior part of the nasal septum. These lesions also have been reported to occur in paranasal sinuses and nasopharynx [5,6].
We experienced two cases of REAH originating from the nasal septum, which were treated by endoscopic surgery, and present their clinical findings and histopathologic features.
CASE REPORTS
Case 1
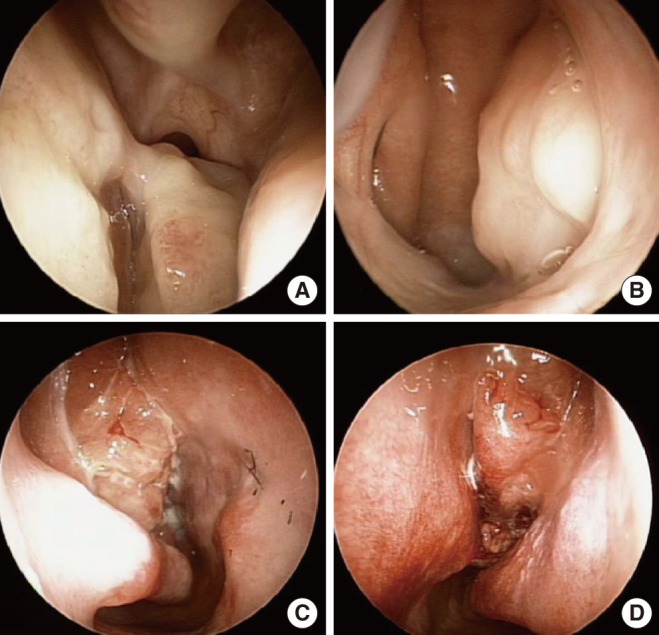
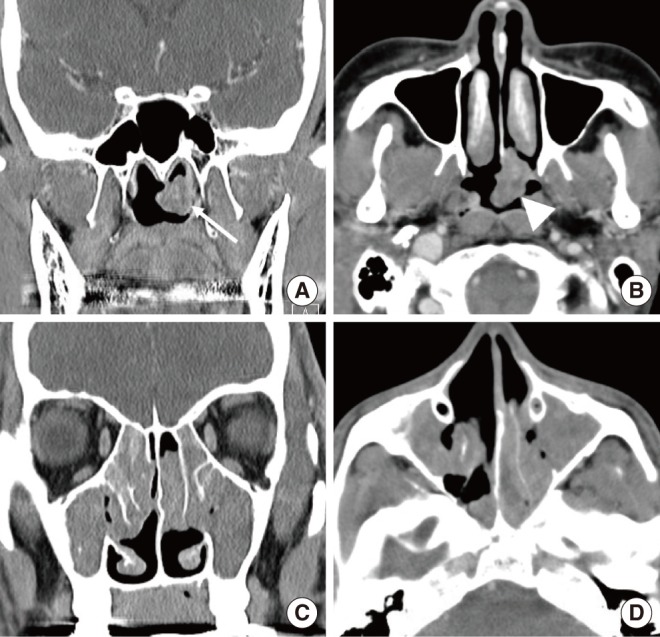
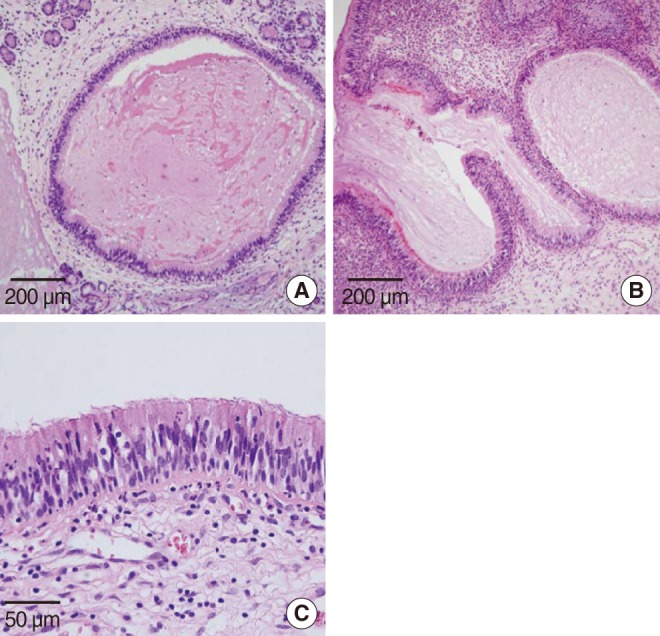
A 50-year-old woman presented with left nasal obstruction for 3 years and had no other associated sinonasal symptoms. The patient denied any past history including chronic rhinosinusitis, alleric rhinitis, and sinonasal operation. Examination with a nasal endoscope revealed a smooth, mucosa-covered, and polypoid mass on the posterior aspect of nasal septum in the left nasal cavity; the mass originated from the posterior part of the septum (Fig. 1A). The mass extended to the right side through the nasopharynx (Fig. 1B). Computed tomography (CT) coronal view scans of paranasal sinuses revealed a left nasopharyngeal mass (Fig. 2A). Axial view CT revealed that the mass was attached to the posterior aspect of the nasal septum (Fig. 2B). A pre-operative punch biopsy of the mass suggested the diagnosis of REAH. Under general anesthesia, intranasal endoscopic excision was performed. The excised specimen measured 23 mm├Ś16 mm├Ś13 mm. On histological analysis, the surface of the lesion was found to comprise pseudostratified, ciliated, columnar epithelium and was composed of proliferated glands lined by ciliated respiratory epithelium. No atypical cells were seen and there was no evidence of metaplasia (Fig. 3A). The pathologic finding was consistent with REAH. The patient tolerated the operation well and there were no complications during the postoperative period. At 1-year follow-up, there was no evidence of recurrence.
Case 2
A 23-year-old man with a history of obstruction of both nasal passages visited our office. Symptoms first developed about 10 years previously. The patient had undergone a nasal polypectomy 7 years before the current presentation. Nasal endoscopy revealed bilateral nasal polyposis in the middle meatus (Fig. 1C, D). A CT scan of the paranasal sinus showed soft tissue density in all sinus cavity and both middle meatus (Fig. 2C, D). A pre-operative punch biopsy of the mass suggested the diagnosis of REAH. Under general anesthesia, functional endoscopic sinus surgery was performed. Left nasal cavity mass originated from posterior aspect of nasal septum and mass was removed without remnant. Pathology of left nasal cavity mass revealed REAH associated with nasal polyposis and right nasal cavity polyp revealed chronic inflammation. There was a glandular proliferation originating from the surface epithelium (Fig. 3B). The gland was lined by ciliated respiratory epithelium (Fig. 3C). There were no postoperative complications. At 1-year follow-up, there was no evidence of recurrence.
DISCUSSION
REAHs are very rare in the sinonasal tract and were first recognized as a distinctive entity by Wenig and Heffner in 1995 [4]. To date, a very limited number of cases have been reported. In the report by the aforementioned authors, the patients included 27 men and four women aged 27 to 81 years (mean age, 58 years). Symptoms varied depending on the location of the lesions and included nasal obstruction, rhinorrhea, headache, hyposmia, anosmia, epistaxis, facial pain, and proptosis [4]. Another report described a case in which the lesion was discovered as a periapical radiolucency during the course of a dental examination, without the typical sinonasal symptoms being apparent [7]. Approximately 70% of REAHs occur in the nasal cavity, the most common site being the posterior nasal septum. Less frequently, the origin is the lateral nasal wall, middle meatus, inferior turbinate, ethmoid and maxillary sinuses, and nasopharynx. The etiology of REAH is still unknown. One of the present patient featured nasal polyposis and had a past medical history of chronic rhinosinusitis. REAH is sometimes associated with nasal polyposis [4]. Cases of REAH associated with nasal polyposis have been reported [1,8]. REAH has clinical presentations, histologic changes, treatment, and behavior similar to inflammatory polyps, suggesting that the development of REAH is induced secondary to the inflammatory process [1]. However, a recent report on the molecular profile of REAH chronicled a mean fractional allelic loss of 31%, a finding that raises the possibility of REAH being a benign neoplasm rather than a hamartoma [9].
CT and magnetic resonance imaging shows no characteristic signals because they vary according to the main element of the hamartoma [10]. One study reported that, compared to normal and nasal polyposis CT scan, REAH significantly enlarges the olfactory cleft width [11].
On gross evaluation, REAHs appear as edematous-appearing polypoid masses. Histologically, the main morphological aspect is a proliferation and accumulation of glands and ducts covered by pseudostratified, ciliated epithelial cells with no metaplastic or atypical changes. Invagination of the repiratory epithelium leading to the glands may be observed. The characteristic glandular components consist of respiratory epithelium originating from the surface epithelium, with an absence of seromucous glands [2]. In contrast, seromucous glands are characterized by the absence of ciliated epithelial cell proliferation, which represents a reactive response often seen in inflammatory nasal polyps [8].
Simple excision is recommended because no malignant potential is recognized for REAH [9]. Because of the limited growth potential of a hamartoma, recurrence is very rare [12]. A misdiagnosis of REAH as either low-grade adenocarcinoma or inverted papilloma would likely result in more aggressive surgical intervention than is needed for the REAH [13]. Therefore it is important to differentiate REAH from other pathologic diseases.