|
 |
- Search
AbstractObjectivesObstructive sleep apnea (OSA) is a disorder characterized by repetitive partial or complete occlusion of the upper airway during sleep that affects quality of life. The aim of this study was to develop the Korean version of the sleep apnea quality of life index (K-SAQLI) and apply it in Korean patients with OSA.
MethodsNinety-three patients with OSA completed the K-SAQLI. Its construct validity and responsiveness were tested by comparing the baseline and change scores obtained in each domain (i.e., daily functioning, social interactions, emotional functioning, and symptoms) using the medical outcome survey-short form 36 (SF-36).
ResultsThe Cronbach ╬▒ coefficients of internal reliability exceeded 0.60 in all the domains (daily functioning, 0.89; social interactions, 0.88; emotional functioning, 0.92; symptoms, 0.67; and total, 0.94). The K-SAQLI had a high test-retest correlation coefficient of 0.73 in the 20 randomized selected patients. The construct validity was confirmed by significant correlations with SF-36 subscale scores.
Obstructive sleep apnea (OSA) is characterized by recurrent episodes of partial or complete upper airway obstruction during sleep. It occurs as combined episodes of apnea and hypopnea that cause sleep fragmentation or excessive daytime sleepiness [1]. The OSA syndrome can lead to heart- and lung-related diseases, as well as neuropsychiatric disorders, by stimulating the autonomic nervous system. It is also highly associated with automobile accidents [2]. OSA is more prevalent among men than among women and occurs mainly in post-middle age men and frequently in women after menopause [3]. There is a report that 1%-5% of the western male population have the OSA condition [4].
Polysomnography (PSG) is the standard test for the diagnosis of OSA [5,6]. However, because OSA can cause clinical symptoms-such as excessive daytime sleepiness, inactivity, difficulty in concentrating and cognitive decline-that cannot be detected using PSG alone, it may be problematic to rely solely on PSG for diagnosing OSA [7]. Therefore, an objective PSG test along with a questionnaire-based assessment of quality of life is useful for evaluating OSA and for clinical decision-making [8].
The Calgary sleep apnea quality of life index (SAQLI), an OSA-specific questionnaire developed in 1998 by Flemons and Reimer [8], is widely used to measure and assess the 4 domains of health-related quality of life that are considered important to OSA patients: daily functioning (11 questions), social interactions (13 questions), emotional functioning (11 questions), and symptoms (5 questions). The Calgary SAQLI was designed for administration by a trained interviewer. Three color-coded cards are used to visually present response options to patients, with each response graded on a 7-point Likert scale [9]. Studies using the English, French, and Chinese versions of the questionnaire, demonstarate that the Calgary SAQLI results reflect the disease-specific quality of life in OSA patients [9-11].
This study aimed to develop the Korean version of the SAQLI (K-SAQLI) and to use it as a tool to assess the quality of life of OSA patients in Korea. For this purpose, we translated the Calgary SAQLI questionnaire into Korean, adapted its questions for use in Korea, and examined its validity and reliability.
After obtaining approval for the K-SAQLI questionnaire from the original author, we asked an English literature scholar to translate the questionnaire into Korean and modified the translation by consulting 8 otolaryngologists and 5 neurologists, all of whom were OSA specialists, about its clinical applicability to patients. The modified version was retranslated into English by a bilingual (English and Korean) Korean-American doctor who did not know about the content of the questionnaire at the time he began translating; we reviewed the retranslation to check if it was consistent with the original version. Then, we conducted a preliminary test on 20 OSA patients using the Korean version and sent the questionnaire to the Korean Language and Culture Center of Gyeongsang National University, along with problems discovered during the test, to have it fully localized into Korean. The Korean version was granted official approval by the original authors after it had been validated through the formal translation and retranslation process and was officially certified for use in this study.
This study included 93 OSA subjects who completed the K-SAQLI and the medical outcome survey-short form 36 (SF-36) questionnaires; the patients were selected from among OSA subjects diagnosed using the PSG at the sleep laboratories of Kyungpook National University Hospital, Kyunghee Medical Center, Korea University Ansan Hospital, Dong-A University Medical Center, and Daegu Catholic University Medical Center. Each questionnaire was administered by a fully trained sleep technologist before conducting the PSG, scored by a skilled sleep technologist who was not informed of the questionnaire results, and reconfirmed by a sleep disorder specialist. The study included patients with a respiratory disturbance index (RDI)Ōēź5 but excluded subjects with severe systemic or psychiatric disease (e.g., bipolar disorder, anxiety neurosis and panic disorder) or patients who refused to give written informed consent to this study. For the test-retest reliability of the K-SAQLI, the 20 subjects randomly selected from the 93 subjects were asked to repeatedly complete the questionnaire at 2- or 3-week intervals.
The questionnaire items used a 7-point Likert scale, in which 1 point means 'very severe' and 7 points meant 'not at all severe.' The mean score for each domain was calculated by dividing the total score per domain by the number of items in the domain. The total score for the K-SAQLI was calculated by dividing the sum of the 4 domain scores by 4. As a result, the mean scores for the domains and the total score for the SAQLI rating ranged from 1 to 7. Three domains-daily functioning, social interactions, and emotional functioning-should not have more than 2 nonresponse items. If there were 1 or 2 nonresponse items in any of the domains, the mean score for the domain was determined by dividing the sum of the responses by the number of items answered. If the number of nonresponses in each domain exceeded 2, then the domain was not scored. In the "symptoms" domain, patients were asked to select up to 5 symptoms; the mean score for this domain is computed by adding selected symptom points and dividing the sum by 5 regardless of the number of symptoms selected.
The SF-36 questionnaire as a measure of overall health status consists of 36 items/questions in 9 domains. In this study, health status was assessed using 8 domains: physical functioning, social functioning, role physical, role emotional, mental health, vitality, body pain, and general health. These 8 domains were used to assess 2 potential physical and mental health components, and the raw score for each domain was linearly transformed to have a value from 0 to 100.
Data quality was assessed by means, standard deviation, ranges, and percentages of patients scoring minimum (floor) and maximum (ceiling) possible scores for the SAQLI. Floor and ceiling effects between 1% and 15% were defined as optimal [12]. In order to assess internal consistency reliability between the scale items, we calculated Cronbach alpha to estimate whether each item of a scale was appropriate for assessing the underlying conception of its scale. To test high internal consistency, we required values of 0.50-0.70 for group comparisons [13]. The intraclass correlation coefficient (ICC) was used as an estimate of test-retest reliability [14] Several calculation modes are possible for the ICC; as we aimed at assessing test-retest reliability, we used the 'one-way-random' mode in SPSS [15]. Although no standard recommendations exist for the ICC; values above 0.7 are usually regarded as confirmation of high test-retest reliability.
Convergent validity was confirmed by the range of correlation coefficients between the individual items and the domains that the items belonged to and discriminant validity was assessed by comparing the correlation coefficients between a domain and the items in the other domains. In addition, a factor analysis of four K-SAQLI domains was conducted to determine the construct validity. The Varimax rotation method was used to perform factor analysis. Construct validity was also tested by the correlations between the corresponding domains of the K-SAQLI and the SF-36. Pearson's correlation coefficients were used to analyze the correlations between the K-SAQLI and SF-36 questionnaires; the significance level was set at P<0.05. Comparisons of continuous SAQLI domain scores among subjects with different RDI categorizations were made by using ANOVA. The SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Between May 2009 and November 2009, a total of 93 OSA patients who completed the K-SAQLI and SF-36 questionnaires were enrolled in the study. This study was conducted with approval from the Institutional Review Board of Kyungpook National University (approval number: KNUH_09-1041), and all subjects signed informed consent forms.
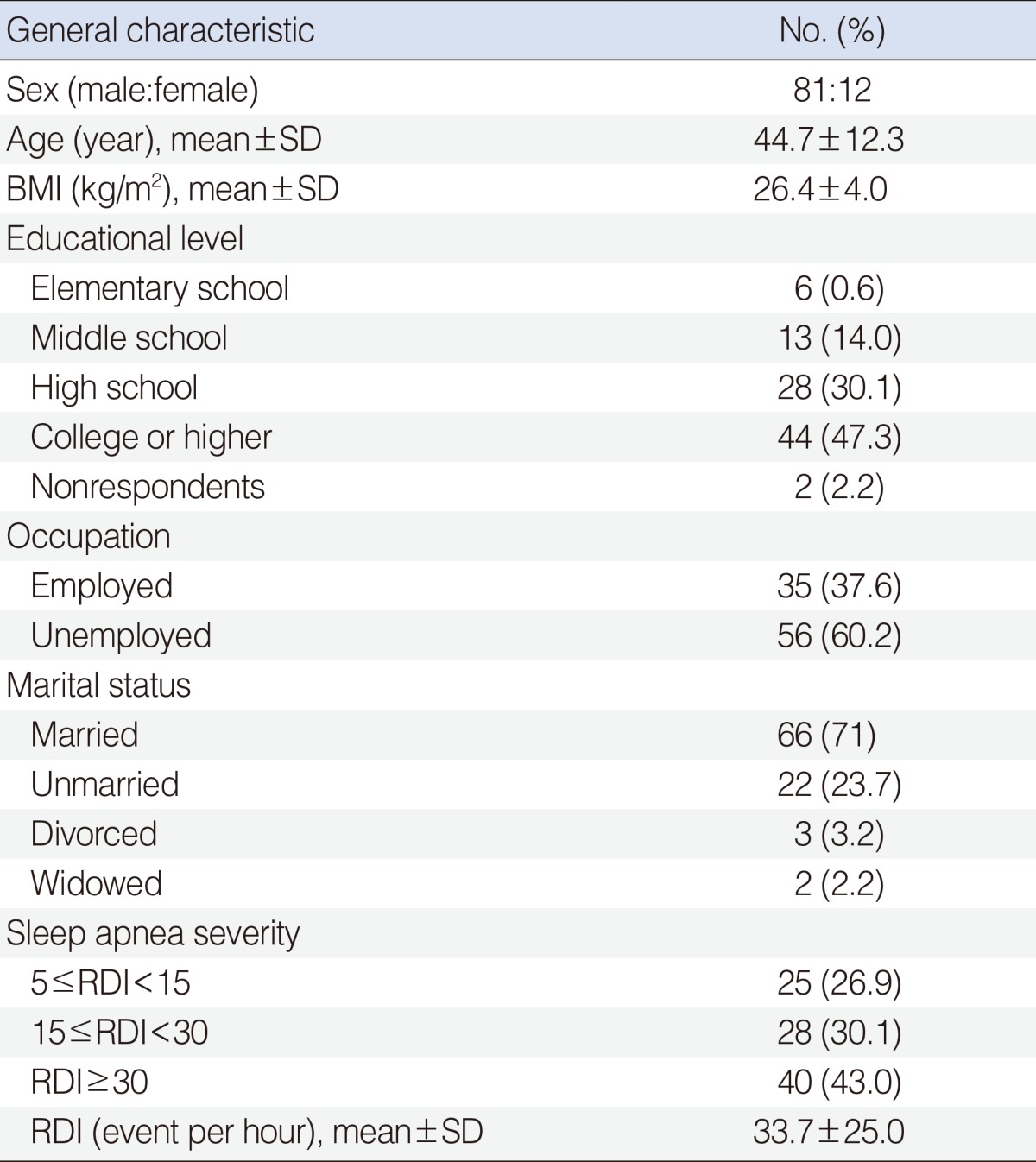
The demographic characteristics of the study subjects are shown in Table 1. The subjects consisted of 81 men (87.1%) and 12 women (12.9%), with a mean┬▒SD age of 44.7┬▒12.3 years and a mean body mass index (BMI) of 26.4┬▒4.0 kg/m2. In terms of educational background, the number of subjects with a college degree or higher was 44 (47.3%), comprising the greatest percentage of the study subjects, followed by high school graduates (30.1%), middle school graduates (14%), elementary school graduates (0.6%), and nonrespondents (2.2%). When OSA was classified as mild (5-15), moderate (15-30), and severe (>30) on the basis of the distribution of RDI scores [13,14], there were 25 mild (26.9%), 28 moderate (30.1%), and 40 severe cases (43.0%).
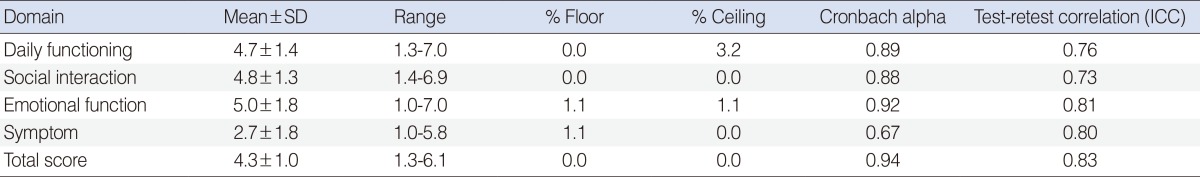
Table 2 shows the means, standard deviations, ranges, and the percentages of patients who obtained the minimum (floor) and maximum (ceiling) scores among the subjects who completed the K-SAQLI.
The score ranges for the K-SAQLI and SF-36 domains are 1-7 and 0-100, respectively; higher scores in each scale indicate better quality of life. In the K-SAQLI results, there were no domains showing a floor effect, and the percentage of patients with the ceiling effect was 3.2% in daily functioning and 1.1% in emotional functioning. No significant floor effects or ceiling effects occurred.
The Cronbach alpha coefficients for each domain were as follows: 0.89 for daily functioning, 0.88 for social interactions, 0.92 for emotional functioning and 0.67 for symptoms, with a total score of 0.94. The reliability coefficients for the individual domains and the total score were greater than 0.60, indicating high internal consistency. In the 20 randomly selected subjects, the test-retest reliability was good, over an intraclass correlation coefficient of 0.73 (Table 2).
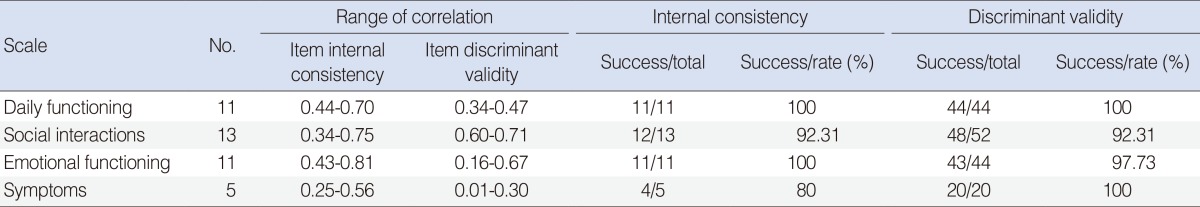
The overall Pearson correlation coefficient ranges between the theoretical construct domains and the items belonging to the domains were high: 0.44-0.70 for daily functioning, 0.34-0.75 for social interactions, 0.43-0.81 for emotional functioning, and 0.25-0.56 for symptoms. The ranges of correlation coefficients between the scores of the items in a specific domain and the other domain scores ranges were 0.34-0.47 for daily functioning, 0.6-0.71 for social interactions, 0.16-0.67 for emotional functioning, and 0.01-0.30 for symptoms, which are relatively low compared to the intraclass correlation coefficients. We assessed the discriminant validity of the questionnaire items on the basis of the calculated coefficients and found an overall success rate exceeding 80% (Table 3).
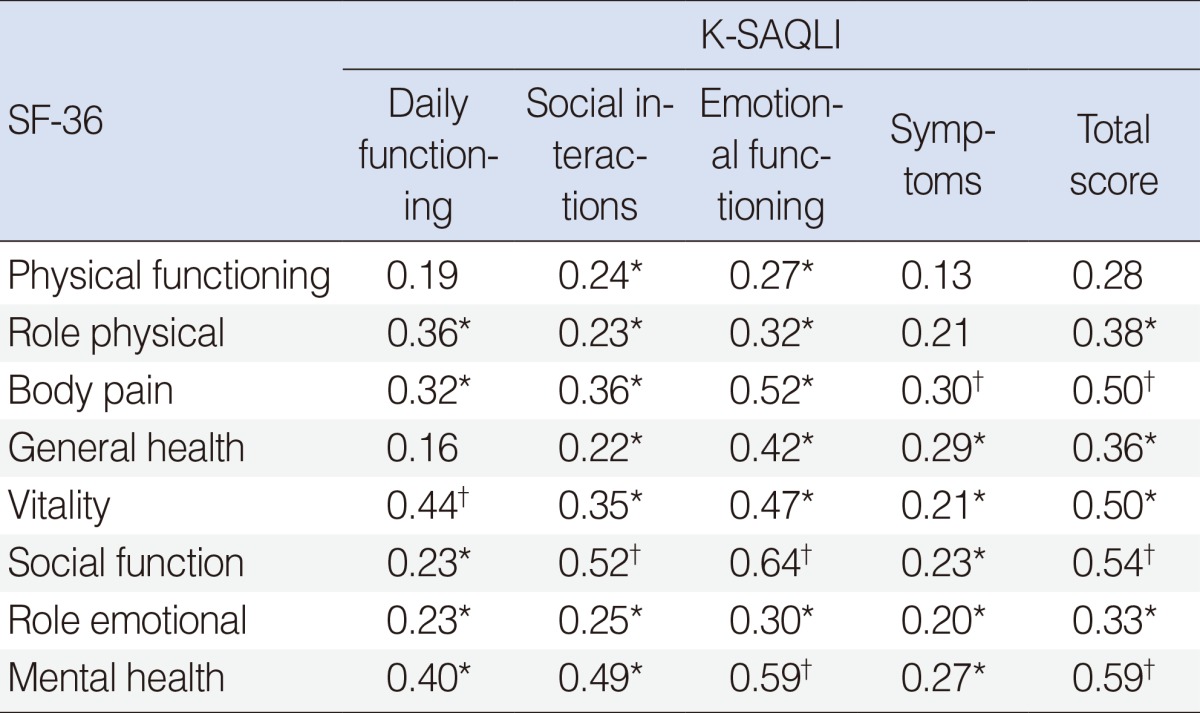
Construct validity was examined by analyzing the interdomain correlations between the K-SAQLI and the SF-36 as measures of quality of life (Table 4). As a whole, the K-SAQLI was significantly correlated with the SF-36 domains, showing high correlations between daily functioning and the SF-36 domains of vitality (╬│=0.44, P<0.001), mental health (╬│=0.40, P<0.05), social interactions and social functioning (╬│=0.52, P<0.001), and emotional functioning, as well as between daily function and the SF-36 domains of social functioning (╬│=0.64, P<0.001) and mental health (╬│=0.59, P<0.001). The domain of symptoms was correlated with the SF-36 domain of body pain (╬│=0.30, P<0.001). The total SAQLI score was significantly correlated with all the domains, except the SF-36 domain of physical functioning (Table 4).
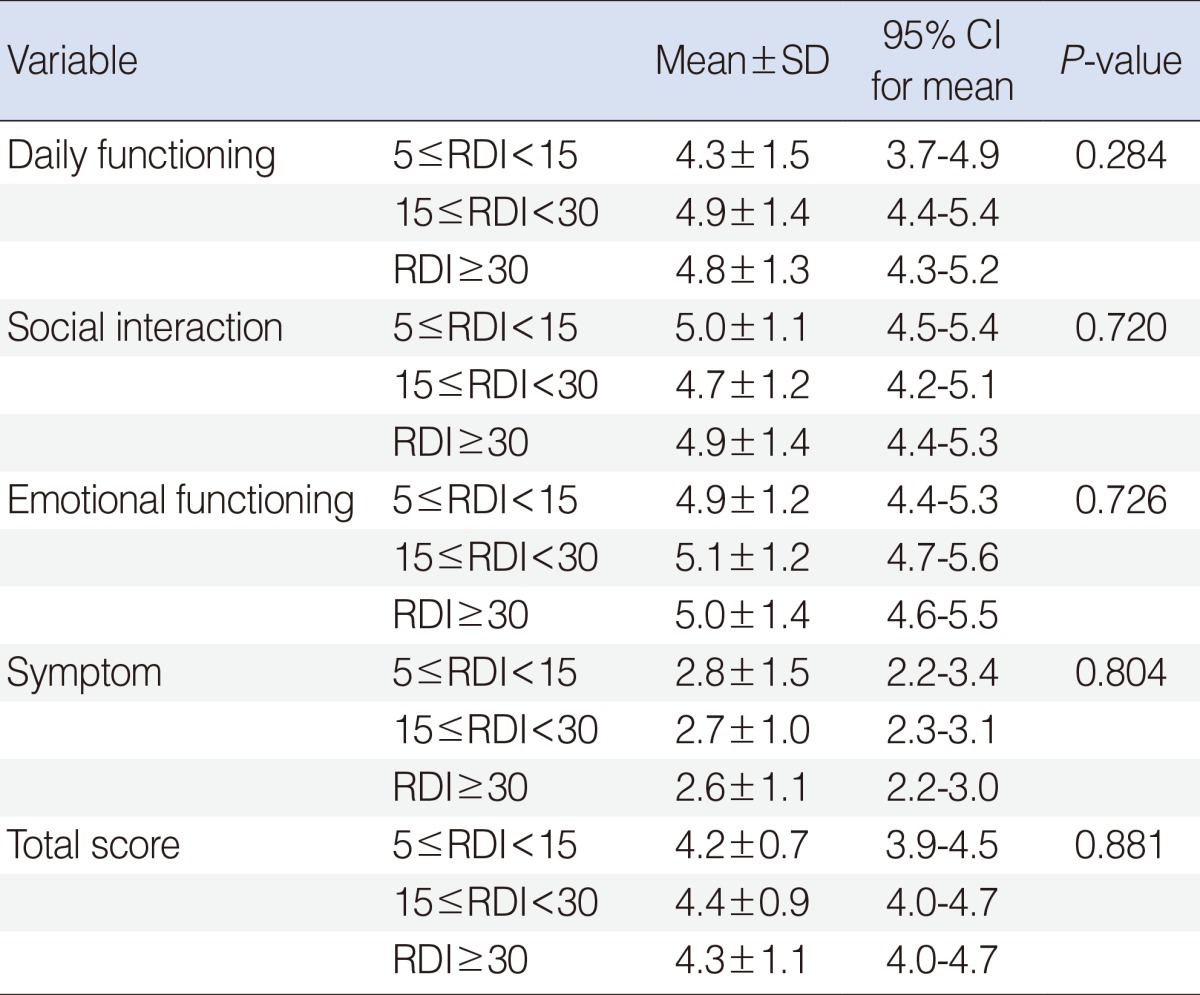
The SAQLI scores of patients subgrouped by RDI are shown in Table 5. There were no significant differences in all domains between individual patient subgroups.
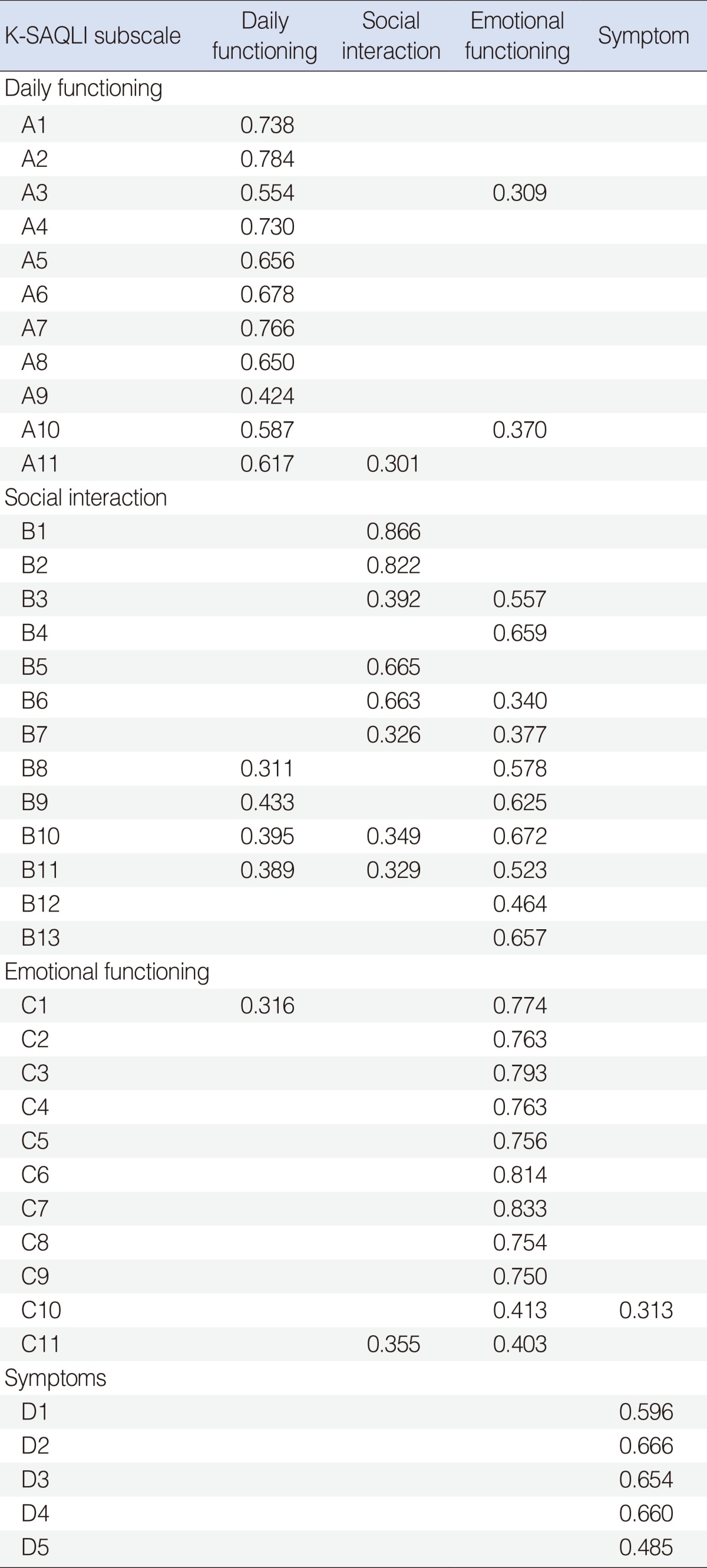
Table 6 shows the factor loadings of the scale items in the 4 K-SAQLI domains. Four factors had significant eigen values greater than 1.0; their descriptive power for the overall variant of K-SAQLI was 54.5%. All of the 11 items in each daily functioning, in emotional functioning, and in symptoms correlated highly with their corresponding domains; however, the 5 items in the symptoms domain poorly correlated with the other domains, which showed significant correlations only with their appropriate domain. The items belonging to the domain of social interactions showed low descriptive power for emotional functioning.
OSA is associated with cerebrovascular and cardiovascular disorders including difficulty concentrating, cognitive decline, daytime headaches, hypertension, arrhythmia, nocturnal cardiac ischemia, myocardial infarction and stroke, and is known to adversely affect quality of life [2,16-18]. Although there are no clear definitions of quality of life, quality of life is known to be influenced by personal characteristics, such as health, aptitude, and mental state. In clinical settings, quality of life is defined as patients' perception and evaluation of the effects that their disease has on their lives. Therefore, assessing quality of life can help a medical teams understand patients with respects to their place and the progress of their diseases, as well as the effects of treatment. Nowadays, the objective of medical care is not only to treat diseases but also to provide a better quality of life and thus maintain physical functioning and mental well-being. This is a concept reflecting changes in the current health-related paradigm. Thus, recent studies of OSA emphasize the importance of patients' quality of life and physical functioning [19].
This study used the K-SAQLI questionnaire through official approval from the original authors after the Korean translation had been validated through the translation and retranslation process. We collected the data from the sleep clinics of 5 university hospitals in Korea, and all study subjects completed the questionnaires, which were administered by well-trained professionals. The Korean patients with OSA easily understood the K-SAQLI, and only a small number of subjects had ceiling and floor score distributions. The relatively low percentage of patients with these distributions was due to the fact that 7 response options were available in each item of the individual domains [9]. Because the K-SAQLI exhibited few ceiling and floor effects, it is also thought to be a more useful quality of life instrument for OSA patients than the SF-36.
The K-SAQLI showed high internal consistency, with the Cronbach ╬▒ coefficients exceeding 0.60 (0.67-0.92) for its domains and total score. These results are similar to those from the questionnaire's English (0.88-0.92), French (0.90-0.94), and Chinese versions (0.79-0.94) [8-11]. The ICC values for assessing test-retest reliability indicated good reproducibility.
In comparisons between the individual K-SAQLI domains and the SF-36 scales, the daily functioning domain of the SAQLI had the highest correlation with the vitality scale of the SF-36. Sleep apnea patients are often obese, feel poorly energized, and lack concentration, which can cause limitations in their physical functioning [9]. In addition, the domains of social interactions and emotional functioning were favorably correlated with all the SF-36 items, because both the SF-36 domains(social functioning and mental health) and SAQLI domains(social interactions and emotional functioning) measure isolated-type symptoms. The symptoms domain also correlated positively with the SF-36 items, other than physical functioning and role physical. The moderate relationships suggest that sleep apnea is associated with fatigue. The total scores and the individual domains favorably correlated with the SF-36 items representing mental rather than physical burden. This was because 24 of the 40 items in the K-SAQLI belong to the social interactions and emotional functioning domains or because mental burden due to difficulty concentrating or memory loss were greater for the patients than physical burdens.
The SAQLI scores were not significantly different between the patient subgroups as categorized by RDI. The other results also found that the SAQLI scores of untreated patients did not correlate with AHI [10,11].
Our factor analysis of the K-SAQLI domains showed good construct in the Korean version. However, the items on social interactions showed mixed patterns for 2 scales (social interactions and emotional functioning). This difference may also reflect nonequivalence of difference in the conception of social interactions between Korean and Canadian cultures or that some items in the social interactions domain were influenced by personal feelings or emotions. The interscale correlation between the social interactions domain and emotional functioning domain was very high (r=0.724, P<0.001), suggesting the possibility of redundancy of items in these 2 domains. Similar results are also found in the Chinese version of the SAQLI questionnaire [9].
This study has some limitations. Owing to the poor patient participation, we could not determine the improvements in quality of life by dividing the subjects who completed the questionnaires into 2 groups-the CPAP-treated and control (untreated with CPAP) groups-or monitor changes in patient conditions. Therefore, future studies need to administer the questionnaires to OSA patients on a continuous basis during the treatment process and to compare the results in a more comprehensive context in the future.
In this study, we translated the Calgary SAQLI questionnaire into Korean and developed the translation into the K-SAQLI questionnaire, with the original author's official approval. The K-SAQLI questionnaire had high levels of internal consistency, test-retest reliability, and construct validity.
In conclusion, the K-SAQLI questionnaire can be a very useful measure of quality of life because it exhibits fewer ceiling and floor effects than other commonly used quality of life questionnaires such as the SF-36.
References1. Redline S, Strohl KP. Recognition and consequences of obstructive sleep apnea hypopnea syndrome. Clin Chest Med. 1998 3;19(1):1-19. PMID: 9554214.
2. Bassiri AG, Guilleminault C. Clinical features and evaluation of obstructive sleep apnea-hypopnea syndrome. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia, PA: Saunders Co; 2000. p. 869-878.
3. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993 4;328(17):1230-1235. PMID: 8464434.
4. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002 5;165(9):1217-1219. PMID: 11991871.
5. Coleman RM, Roffwarg HP, Kennedy SJ, Guilleminault C, Cinque J, Cohn MA, et al. Sleep-wake disorders based on a polysomnographic diagnosis: a national cooperative study. JAMA. 1982 2;247(7):997-1003. PMID: 7057593.
6. Roth T, Hartse KM, Zorick F, Conway W. Multiple naps and the evaluation of daytime sleepiness in patients with upper airway sleep apnea. Sleep. 1980;3(3-4):425-439. PMID: 6111835.
7. Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: a new approach. Psychophysiology. 1973 7;10(4):431-436. PMID: 4719486.
8. Flemons WW, Reimer MA. Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med. 1998 8;158(2):494-503. PMID: 9700127.
9. Mok WY, Lam CL, Lam B, Cheung MT, Yam L, Ip MS. A Chinese version of the Sleep Apnea Quality of Life Index was evaluated for reliability, validity, and responsiveness. J Clin Epidemiol. 2004 5;57(5):470-478. PMID: 15196617.
10. Lacasse Y, Godbout C, Series F. Independent validation of the Sleep Apnoea Quality of Life Index. Thorax. 2002 6;57(6):483-488. PMID: 12037222.
11. Flemons WW, Reimer MA. Measurement properties of the calgary sleep apnea quality of life index. Am J Respir Crit Care Med. 2002 1;165(2):159-164. PMID: 11790647.
12. McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995 8;4(4):293-307. PMID: 7550178.
13. Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
14. Streiner DL. Learning how to differ: agreement and reliability statistics in psychiatry. Can J Psychiatry. 1995 3;40(2):60-66. PMID: 7788619.
15. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979 3;86(2):420-428. PMID: 18839484.
16. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999 8;22(5):667-689. PMID: 10450601.
17. Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, et al. Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med. 1997 8;157(15):1746-1752. PMID: 9250236.
18. Strollo PJ Jr, Rogers RM. Obstructive sleep apnea. N Engl J Med. 1996 1;334(2):99-104. PMID: 8531966.
19. Yang EH, Hla KM, McHorney CA, Havighurst T, Badr MS, Weber S. Sleep apnea and quality of life. Sleep. 2000 6;23(4):535-541. PMID: 10875560.
|
|
|||||||||||||||||||||||||||||||||||||||||||