 |
 |
- Search
AbstractObjectivesHead and neck reconstruction is still challenging in terms of esthetic and functional outcomes. This study investigated the feasibility of the angular branch-based scapular tip free flap (STFF).
MethodsThis was a retrospective study of 17 patients undergoing maxillectomy and mandibulectomy and either primary or secondary reconstruction by STFF. This study included surgical, esthetic, and functional outcomes, and detailed data are presented regarding the flap, such as pedicle length, size of the harvested bone, and failure rate. Medical photographs were used to estimate the esthetic outcome, and computed tomography was used to check the flap status postoperatively.
ResultsThe data were collected from April 2013 to April 2014. Eight patients underwent maxillary reconstruction, and nine underwent mandibular reconstruction. Maxillary defects usually included unilateral alveolar structures and the palate; mandibular defects were usually those involving mandibular angle and short segment. Vein grafting was not required in any of the patients. Flap failure occurred in one of the 17 patients (5.9%) with successful reconstruction after revision. Of the eight maxillectomy patients, orbital revisions for diplopia after maxillary reconstruction were performed in two patients (25%), and oroantral fistula repair was performed in one patient (12.5%).
ConclusionThis study demonstrated the reconstructive advantages of the angular branch-based STFF, long pedicle, low flap failure, 3-dimensional nature of bone and soft tissues (chimeric flap), and small rate of donor site morbidity with free ambulation. This flap is an excellent option for use in complex three-dimensional head and neck reconstruction.
The defects after maxillectomy and mandibulectomy are quite similar in terms of esthetic and functional significance, and are still challenging for reconstruction. These defects are usually reconstructed using an osseous free flap with or without soft tissue components, because defects include the bone with intraoral and extraoral structures simultaneously. Common reconstruction options are the fibula and iliac crest. These conventional options have disadvantages, however, such as short pedicle, donor site morbidity, limited ambulation, and unfavorable complex three-dimensional (3D) head and neck reconstruction [1].
Therefore, reconstructive surgeons have used the lateral scapular border free flap based on the circumflex scapular artery [23]. This technique allows ambulation without limitations soon after the operation. Furthermore, this flap has a chimeric nature, independently mobile harvested skin paddles, muscles (teres major, latissimus dorsi [LD], serratus), and lateral scapular bone [34]. These characteristics facilitate delicate 3D reconstruction for composite defects of the head and neck. However, the lateral scapular border free flap has several disadvantages, including short vascular pedicle and morphological dissimilarity to the bone of the mandible and maxilla [56].
A number of technical developments have been made to overcome these disadvantages. The scapular tip free flap (STFF) based on the angular branch of the thoracodorsal artery has been modified from the traditional scapular free flap. Coleman and Sultan [7] reported a series of cadaveric and surgical dissections with eight cases of STFF reconstruction in 1991.
The STFF has additional advantages over the traditional lateral bone scapular border free flap, with increased pedicle length and morphological similarity to the native mandible angle, maxilla, and palate. These improvements facilitate a reduced rate of vein grafting during revascularization of the flap, and make delicate flap fabrication possible without additional osteotomies [568910].
This report presents the surgical, esthetic, and functional outcomes, and details data regarding the flap, such as pedicle length, size of the harvested bone, and failure rate in a series of 17 patients treated with a STFF.
A retrospective review of all patients undergoing STFF for head and neck reconstruction at Samsung Medical Center from April 2013 to April 2014 was performed. Data collected included age, sex, defect site, pathology, previous treatment, and time of reconstruction. The patients were divided into two groups (i.e., patients undergoing maxillary reconstruction and those undergoing mandibular reconstruction). The surgical findings, postoperative complications, imaging studies, and medical photographs were also collected in both groups, and all of the patients provided informed consent for the publication of facial photographs.
We examined the surgical findings, including defect type, size of harvested scapular bone and pedicle, recipient vessels, complications, and esthetic outcome.
The short-term and long-term complications were reviewed from medical charts retrospectively. We examined the complications of donor and reconstruction sites, such as bleeding, fistula, infection, flap failure, and diplopia.
The physician graded the esthetic results from photographs of the patients that were taken 1 month after surgery. Patients estimated their shoulder function during daily activities after the operation.
The patient was placed in the 30┬░ lateral decubitus position with a rolled-up towel under the inferolateral border of the LD. This position allows a two-team approach in selected cases for simultaneous tumor resection and flap harvesting [13]. During the harvest procedure, the shoulder is fully adducted and fixed in position, which rotates the scapula upward and outward, and secures the operating field. After positioning, an S-shaped cutaneous incision is made from the midaxilla along the lateral border of the LD, and towards the scapular tip. The first step involves exposing the dorsal aspect of the LD, mobilizing it from the scapular border and the teres major (Fig. 1A). This procedure should be accomplished first to facilitate pedicle management (Fig. 1B). The vascular pedicle must be manipulated carefully because its course is variable between individuals. The pedicle was identified at the origin of the thoracodorsal artery from the subscapular vessels, and then traced down the course of the thoracodorsal artery until the emerging branches to the serratus anterior, teres major, and angular branch (Fig. 1C). If the parascapular skin is needed for the reconstruction, the circumflex scapular artery should be preserved. Similarly, if any muscular structure is also needed, such as the teres major or serratus anterior, vascular branches to these muscles should be saved. When the pedicle had been fully identified and mobilized, osteotomy of the scapular tip bone was performed according to the defect size (Fig. 1D). The size of the bone should be carefully assessed before osteotomy, because further osteotomy in the scapular tip could lead to flap failure. After flap harvest, the remaining teres major muscle was fixed to the remnant scapular bone to facilitate the recovery of muscle function, and to prevent seroma and hematoma (Fig. 1E). Three holes were drilled in the remaining scapular bone, and the teres major muscle was fixed to the scapular bone via these holes using 3-0 nylon sutures. In all of the patients, primary closure of the donor site was achieved, and a sling was applied to the arm until 1 week postoperatively.
We used 3D midface rapid prototype model (replica) for delicate maxillectomy and reconstruction. The reconstruction plate (Synthes CMF; Synthes, Mississauga, ON, Canada) was prefabricated on a patient-specific rapid prototype model. If orbital reconstruction was needed, titanium mesh (Synthes CMF) was prefabricated using the rapid prototype model (Fig. 2A). The harvested scapular tip bone was placed vertically in the malar area to reconstruct the zygomatic bone and maxilla in all cases. The muscular component was positioned at the palate for reconstruction and obliteration of the defect cavity. The scapular tip bone was fixed at the premaxilla and maxillary process of the zygomatic bone with the titanium plate, and the prefabricated titanium mesh was placed on the bony defect of the orbital rim and stably positioned at the remained surrounding bony structures (Fig. 2B). The flap pedicle was tunneled through the buccal space deep to the facial nerve over the mandible and anastomosed with a single artery and vein. The superior thyroidal artery and internal jugular vein were usually used for revascularization.
A patient-specific 3D facial bone rapid prototype model was made, and the reconstruction plate was prebent on this model preoperatively in a manner similar to maxillary reconstruction (Fig. 2C). The mandibulectomy involved oral cavity mucosa with or without skin defect. The scapular tip bone was placed at the mandibular defect, and the muscle could be positioned at the oral cavity mucosal defect (Fig. 2D). In cases requiring facial skin resection, the skin was harvested as a chimeric flap to cover the skin defect. After positioning the flap, a prefabricated reconstruction plate was used for fixation of the scapular bone at the remaining mandible.
The clinical data are summarized in Table 2. Eight patients underwent reconstruction via Weber-Fergusson incision with Lynch extension (4 males, 4 females; median age, 51 years; range, 41 to 66 years). The scapular tip bone was used for malar reconstruction (vertically inset at the anterior maxillary wall) in all of the cases. Two patients had class Ib f, two had class II f, two had class III, one had class III fz, and one patient had class Ib f defects. The distribution of pathological subtypes was as follows: squamous cell carcinoma, n=2; adenoid cystic carcinoma, n=3; adenocarcinoma, n=1; chondrosarcoma, n=1; melanoma, n=1. Case No. 1 received concurrent chemoradiotherapy previously, and case No. 2-6 had no previous treatment before surgery. Case No. 1-6 simultaneously underwent wide tumor excision and reconstruction. Case No. 7 and 8 underwent delayed reconstruction with confirmation of no evidence of tumor recurrence for 5 years.
The reconstruction data are listed in Table 3. The median size of the scapular tip bone was 4.5 cm (long axis; range, 3.9 to 5.0 cm)├Ś1.5 cm (short axis; range, 1.0 to 2.5 cm). The median pedicle length was 10.8 cm (range, 8.2 to 13 cm), and there was no need for vein grafting in revascularization of the flap in any of the patients. Six patients had orbital floor defects (subclass f defect) that were reconstructed with titanium mesh. The LD muscles were used in all cases for reconstruction of the maxillary cavity or hard palate. The superior thyroidal artery and internal jugular vein were used for revascularization in six cases, the superficial temporal artery and vein were used in one case, and the facial artery and lingual vein were used in one case.
Two patients (cases No. 1 and 8) suffered from diplopia postoperatively, case No. 1 was corrected by orbital floor reconstruction with another titanium mesh, and case No. 8 underwent medial canthopexy. Case No. 4 had flap failure and underwent revision surgery with a contralateral STFF. Case No. 7 developed oroantral fistula postoperatively despite curettage and suturing of the fistula several times, and was finally treated with an anterolateral thigh free flap.
Esthetic outcomes 1 month after reconstruction were excellent in three cases, good in two cases, and fair in three cases. The oral cavity defects that were reconstructed with a muscle flap usually achieved complete mucosalization within 2 months after surgery. Medical photographs of case No. 1 are shown in Fig. 3.
The reconstruction data are summarized in Table 4. Nine patients underwent mandibular reconstruction via the lower cheek approach with or without lip splitting (6 males, 3 females; median age, 54.2 years; range, 34 to 79 years). The distribution of pathological subtypes was as follows: squamous cell carcinoma, n=7; osteosarcoma, n=1; chondrosarcoma, n=1. Three patients had retromolar trigone cancer, two had buccal cancer, two had mandible bone tumor, and one had gingiva cancer. Seven patients underwent salvage surgery, and two patients had no history of prior treatment. All of the patients simultaneously underwent wide tumor excision and reconstruction.
The reconstruction data are summarized in Table 5. Three patients (case No. 1, 2, 4) suffered from oral cavity mucosal dehiscence and bone exposure. Case No. 1 required repair operation only, and the others responded well to conservative management. All of the patients had successful free flap reconstruction without failure. Esthetic outcomes 1 month after reconstruction were considered excellent in four cases, good in two cases, and fair in three cases. Similar to maxillary reconstruction, the reconstructed oral cavity defects healed within 2 months after surgery. Medical photographs of case No. 15 are presented in Fig. 4.
There were no donor site complications, such as infection, hematoma, or dehiscence, in any case in the present series. All patients except case 4 showed recovery of shoulder function after 1 month without restriction of daily activities. Case No. 4 underwent bilateral scapular tip harvest because of flap failure, and had difficulties in internal rotation of both upper extremities.
There are morphological similarities between the anterior maxillary wall, mandible angle, and the scapular tip. Therefore, STFF could provide relatively good esthetic outcomes compared to other free flaps in head and neck reconstruction. These similarities reduced the further osteotomy of the harvested scapular tip bone. The harvested scapular tip bone could be used in these areas without osteotomies.
In previous reports of maxillary reconstruction with STFF, the bony component of the flap was placed either horizontally to the palatoalveolar complex or vertically to the anterior midface. The scapular tip is usually positioned vertically in the case of class I or II defects. Otherwise, it is oriented horizontally in the case of class III defects [689]. However, we positioned the bony components vertically as malar position in all cases, even in class III defects. This could prevent midfacial depression, which could occur long after surgery. If the scapular tip bone was too small to cover the defect of the anterior wall of the midface, abundant soft tissues, such as LD or teres major muscle, could support the defect site together.
In terms of mandibular reconstruction, we usually use STFF for mandibular angle reconstruction. The angle and lateral body of the mandible are the best candidates for STFF because of its morphological similarity [10].
The STFF is an excellent option for use in midface and mandible reconstruction, which require a long pedicle length. The pedicle length was up to 17 cm in previous reports [10141516]. In our series, the average pedicle length was 10.0 cm (range, 7.7 to 13.1 cm), and no vein grafting was needed in any of the cases.
We used the STFF to reconstruct short segment of the mandible and maxilla. In our series, the size of the harvested scapular tip bone averaged 4.6 cm, with the longest section measuring 7.7 cm. The segmental mandibular defects were usually less than 8 cm, and the scapular tip bone was sufficient for reconstruction [10].
In terms of functional outcome of reconstruction, none of the patients in our series suffered from any swallowing difficulty or velopharyngeal reflux. When performing maxillary reconstruction, we harvested abundant muscular components, such as LD or teres major muscle, and placed the muscle flap at the hard palate and maxillary cavity. We positioned the bulky LD muscle at the hard palate defect, and this flap shrunk and was mucosalized completely within 2 months in all of the cases. The LD muscle supported the oral cavity and velopharynx in swallowing and phonation.
Controversy still exists regarding whether maxillectomy defects should be reconstructed or obturated [817]. Clark et al. [8] used both obturation and reconstruction to achieve optimal functional outcomes, and Rogers et al. [18] suggested that as the defect increases, the functional outcome and patient satisfaction are diminished with obturation only. However, we achieved successful functional outcomes without obturation. With mandibular reconstruction, which inevitably included the oral cavity defect, muscular components of STFF were used for covering the oral cavity mucosal defect and complete mucosalization was achieved in all cases. This enabled early oral feeding and good functional restoration.
There have been reports of donor site complications in 5%-10% of cases of STFF, including seroma, infection, wound dehiscence, and shoulder dysfunction [468]. We prevented these complications through additional techniques. After harvesting, we attached the remained teres major muscle to the remnant scapular bone with nonabsorbable sutures, and applied a sling to the arm for 1 week postoperatively. These procedures reduced dead space from the large volume of harvested bone and soft tissues, and facilitated the recovery of muscle function and prevented seroma and hematoma.
The major advantage of STFF is its chimeric nature, which facilitates 3D complex head and neck reconstruction. Conventional fibular flaps and iliac crest flaps have limitations in rotation of each flap component, soft tissue, skin, and bone. Patients treated with conventional osseous flaps suffer from delayed ambulation, but the STFF enabled free ambulation. The scapula is composed of light and thin cortical bone in its medial portion, and its vascular structure has a low rate of atherosclerosis. These characteristics ensure flap stability and viability [1192021]. Abundant soft tissues composed of various muscles and skin could be used for palatal bone, oral cavity mucosa, or skin defects and achieve good esthetic and functional recovery [5810].
The main indications for this free flap system reported to date are classes II and III maxillary defects according to the Okay classification, with or without the orbital content defect [58]. However, we suggest that malar setting of the scapular tip and palatal setting of LD muscles could result in successful reconstruction of more extensive defects. In mandibular reconstruction, STFF was indicated in the short segment of bony defects less than 8 cm involving the mandibular angle. The extent of skin, mucosa, and muscular defects may not limit the indication of STFF, because it could involve large amounts of soft tissue components.
In conclusion, this study demonstrated the reconstructive advantages of angular branch-based STFF, including a long pedicle from the thoracodorsal artery to the angular branch, low flap failure rates, the 3D nature of the scapular tip and soft tissue components, and low rates of donor site morbidity with free ambulation. STFF in head and neck reconstruction could improve the quality and success rate of complex reconstructions without vein grafts and multiple separate donors. STFF should be considered the first choice for patients in whom early mobilization is critical and defects are complex and extensive, including bone and large muscles.
ACKNOWLEDGMENTSThis research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HI14C2215).
CONFLICT OF INTERESTCONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported. References1. Dowthwaite SA, Theurer J, Belzile M, Fung K, Franklin J, Nichols A, et al. Comparison of fibular and scapular osseous free flaps for oromandibular reconstruction: a patient-centered approach to flap selection. JAMA Otolaryngol Head Neck Surg. 2013 3;139(3):285-292. PMID: 23657276.
2. Moukarbel RV, White JB, Fung K, Franklin JH, Yoo JH. The scapular free flap: when versatility is needed in head and neck reconstruction. J Otolaryngol Head Neck Surg. 2010 10;39(5):572-578. PMID: 20828522.
3. Gibber MJ, Clain JB, Jacobson AS, Buchbinder D, Scherl S, Zevallos JP, et al. Subscapular system of flaps: an 8-year experience with 105 patients. Head Neck. 2015 8;37(8):1200-1206. PMID: 24800735.
4. Valentini V, Gennaro P, Torroni A, Longo G, Aboh IV, Cassoni A, et al. Scapula free flap for complex maxillofacial reconstruction. J Craniofac Surg. 2009 7;20(4):1125-1131. PMID: 19506522.
5. Miles BA, Gilbert RW. Maxillary reconstruction with the scapular angle osteomyogenous free flap. Arch Otolaryngol Head Neck Surg. 2011 11;137(11):1130-1135. PMID: 22106238.
6. Piazza C, Paderno A, Taglietti V, Nicolai P. Evolution of complex palatomaxillary reconstructions: the scapular angle osteomuscular free flap. Curr Opin Otolaryngol Head Neck Surg. 2013 4;21(2):95-103. PMID: 23385785.
7. Coleman JJ 3rd, Sultan MR. The bipedicled osteocutaneous scapula flap: a new subscapular system free flap. Plast Reconstr Surg. 1991 4;87(4):682-692. PMID: 2008466.
8. Clark JR, Vesely M, Gilbert R. Scapular angle osteomyogenous flap in postmaxillectomy reconstruction: defect, reconstruction, shoulder function, and harvest technique. Head Neck. 2008 1;30(1):10-20. PMID: 17636540.
9. Pagedar NA, Gilbert RW, Chan H, Daly MJ, Irish JC, Siewerdsen JH. Maxillary reconstruction using the scapular tip free flap: a radiologic comparison of 3D morphology. Head Neck. 2012 10;34(10):1377-1382. PMID: 22287228.
10. Yoo J, Dowthwaite SA, Fung K, Franklin J, Nichols A. A new angle to mandibular reconstruction: the scapular tip free flap. Head Neck. 2013 7;35(7):980-986. PMID: 22847980.
11. Okay DJ, Genden E, Buchbinder D, Urken M. Prosthodontic guidelines for surgical reconstruction of the maxilla: a classification system of defects. J Prosthet Dent. 2001 10;86(4):352-363. PMID: 11677528.
12. Deleyiannis FW, Rogers C, Lee E, Russavage J, Gastman B, Dunklebarger J, et al. Reconstruction of the lateral mandibulectomy defect: management based on prognosis and location and volume of soft tissue resection. Laryngoscope. 2006 11;116(11):2071-2080. PMID: 17075408.
13. Nishimura T, Furukawa M, Koshima I. Scapular bone flap harvests of patients in a supine position. Laryngoscope. 2004 6;114(6):1130-1132. PMID: 15179227.
14. dos Santos LF. The vascular anatomy and dissection of the free scapular flap. Plast Reconstr Surg. 1984 4;73(4):599-604. PMID: 6709742.
15. Seneviratne S, Duong C, Taylor GI. The angular branch of the thoracodorsal artery and its blood supply to the inferior angle of the scapula: an anatomical study. Plast Reconstr Surg. 1999 7;104(1):85-88. PMID: 10597678.
16. Seitz A, Papp S, Papp C, Maurer H. The anatomy of the angular branch of the thoracodorsal artery. Cells Tissues Organs. 1999 7;164(4):227-236. PMID: 10436331.
17. Brown JS, Jones DC, Summerwill A, Rogers SN, Howell RA, Cawood JI, et al. Vascularized iliac crest with internal oblique muscle for immediate reconstruction after maxillectomy. Br J Oral Maxillofac Surg. 2002 6;40(3):183-190. PMID: 12054706.
18. Rogers SN, Lowe D, McNally D, Brown JS, Vaughan ED. Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral Maxillofac Surg. 2003 2;61(2):174-181. PMID: 12618993.
19. Corbitt C, Skoracki RJ, Yu P, Hanasono MM. Free flap failure in head and neck reconstruction. Head Neck. 2014 10;36(10):1440-1445. PMID: 24038609.
20. van Gemert JT, van Es RJ, Rosenberg AJ, van der Bilt A, Koole R, Van Cann EM. Free vascularized flaps for reconstruction of the mandible: complications, success, and dental rehabilitation. J Oral Maxillofac Surg. 2012 7;70(7):1692-1698. PMID: 22079062.
Fig.┬Ā1Surgical procedures used for harvesting a scapula tip free flap. (A) Identification of the latissimus dorsi and teres major muscle (asterisk). (B) Identification of the thoracodorsal vessels, branch to the latissimus dorsi muscle (asterisk). (C) Identification of the angular branch to the scapular tip (arrow). (D) Harvesting of the scapular tip with the teres major muscle, cut surface of the scapula tip bone is shown (arrowhead). (E) Anchoring of the teres major muscle on the remnant scapula angle. (F) Harvested scapula tip and latissimus dorsi muscle as a chimeric flap.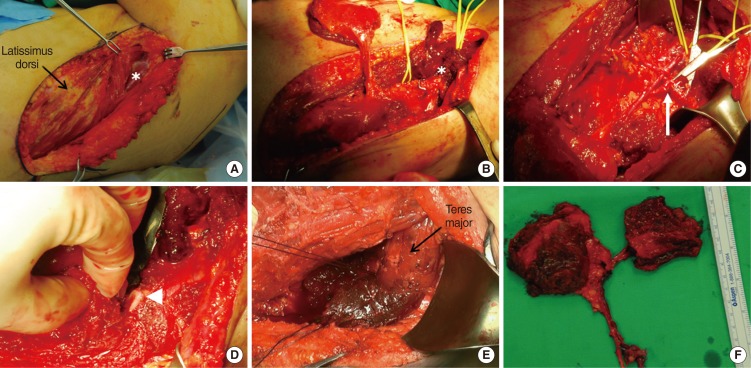
Fig.┬Ā2(A) Three-dimensional printed facial bone rapid prototype and preoperative fabrication of titanium mesh. (B) Reconstruction of the maxillary defect. The scapular tip bone was fixed at the premaxilla and maxillary process (asterisk), and the latissimus dorsi muscle was positioned at the defect in the hard palate and maxillary cavity (arrow). Inferomedial orbital rim reconstructed with titanium mesh (arrowheads). (C) Three-dimensional printed mandible and preoperative fabrication of the titanium plate. (D) Reconstructed mandibular angle defect with the scapula tip free flap fixed with a titanium plate (arrowheads). The latissimus dorsi muscle was placed at the oral mucosal defect (asterisk).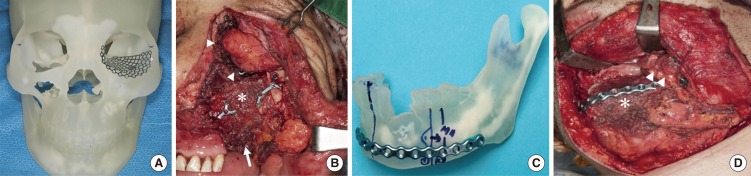
Fig.┬Ā3Facial photographs of a patient who underwent maxillary reconstruction (case No. 1), taken preoperatively (A), and 1 (B), 2 (C), and 6 weeks (D) postoperatively. Photographs of the palatal mucosalization, taken 1 week (E), 1 month (F), and 2 months (G) postoperatively.
Fig.┬Ā4The facial photographs of a patient who underwent mandibular reconstruction (case No. 15), taken preoperatively (A), and 1 (B), 2 (C), and 6 weeks (D) postoperatively. Photographs of the retromolar and buccal mucosalization, taken 1 week (E), 1 month (F), and 2 months (G)postoperatively.
Table┬Ā1.Table┬Ā2.Clinical data of maxillary reconstruction patientsTable┬Ā3.Maxillectomy reconstruction dataTable┬Ā4.Clinical data of mandibular reconstruction patientsTable┬Ā5.Mandibular reconstruction data |
|
||||||||||||||||||||||||||||||||||||||||||







