INTRODUCTION
Since Herman Boerhaave first elucidated the pathology of esophageal perforation after vomiting in 1,724, the spontaneous transmural perforation of the esophagus has referred to as Boerhaave's syndrome. In fact, this nearly always results from an identifiable increase in the intraluminal esophageal pressure commonly after excessive vomiting and retching (1). The most common anatomical location of the tear in Boerhaave's syndrome is at the left posterolateral wall of the lower third of the esophagus, 2-3 cm before the stomach. So, esophageal perforation is commonly associated with high morbidity and mortality (2). However, spontaneous perforation of the pharynx or cervical esophagus is extremely rare and the pathophysiology may be some different from that of Boerhaave's syndrome (3-6). The following report was a case of spontaneous pharyngeal rupture after forceful vomiting. This is presented with a review of literature on the possible mechanisms and management comparing with classic Boerhaave's syndrome.
CASE REPORT
A 20-yr-old man attended an emergency room (ER) with pain in the throat, neck, and anterior chest. He also complained of pain on swallowing. The patient had suffered from common cold for 3 days. He had the recollection of forceful vomiting after lunch and instant beginning to have neck and chest pain. Three hours later, the pain and neck swelling went to worse and then, he visited the ER. He had no history of instrumentation, cervical trauma, or having eaten anything sharp.
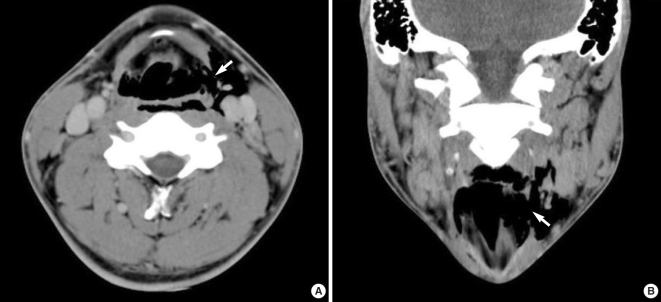
On initial examination, the patient seemed to be anxious but not dyspneic. His vital signs were stable with no fever. There was crepitus in the left side of neck on palpation. Endoscopic examination showed the erythematous swelling of vallecula, aryepiglottic fold, arytenoid on the left side and the immobility of the left vocal fold. There were found some blood clots in the left lateral pharyngeal wall. Gastrografin esophagography revealed a small leakage from the left lateral wall of the oropharynx on pre-swallowing images but no perforation of the esophagus (Fig. 1). Computed tomography (CT) showed a laceration of the left lateral wall of oro- and hypo-pharynx, associated with emphysema around the pharynx and esophagus from the skull base to the upper mediastinum (Fig. 2). The air collections were judged as a result from a tear of the lateral pharyngeal wall. However, the chest CT scans showed no emphysema in the thorax. In addition, there were found no potential underlying causes of the pharyngeal perforation, such as ulceration, diverticulum, or malignancies, on radiological and endoscopic examinations.
Then, broad-spectrum antibiotics and analgesics were administered. A nasogastric tube was passed and feeding commenced from the 3rd day after the rupture. Daily physical and radiographic examinations revealed gradual absorption of the subcutaneous emphysema with no further aggravation. A repeat gastrografin swallow examination revealed no leaks from the pharynx or the esophagus at 7 days after admission. The feeding tube was removed and diet slowly introduced without any problems. CT confirmed that the air collections had disappeared and the tear had changed a fibrotic adhesion and the supraglottic swelling dramatically subsided when the patient was discharged from hospital at 10 days after admission. The immobility of the left vocal fold recovered within one month.
DISCUSSION
Perforation of the pharynx or esophagus most commonly occurs after instrumentation or foreign body ingestion (7-9). The remarkable increase in diagnostic and therapeutic endoscopy has made instrumentation the most common cause of esophageal perforation (9). The perforations can be iatrogenic but also occur spontaneously. Spontaneous rupture of the pharynx or esophagus is a rare condition and the tear is commonly at the lower third of the esophagus. The site is typically an area of natural narrowing, at the level of the aortic arch, the carina or left atrium, or at the esophagogastric junction (1). The pyriform sinus is also at risk because of the absence of a reinforcing longitudinal muscle layer (9). The mechanism of spontaneous pharyngeal or cervical esophageal perforation is thought to involve a sudden large increase in pharyngeal or upper esophageal pressure resulted in rupture of weak wall. This also involves a sudden rise in intraluminal pressure against closed vocal folds most commonly following forceful retching, vomiting, or nose blowing (3-5). In the present case, the rupture site was from the lateral oropharyngeal wall to the upper hypopharynx, which is higher than that of previous reports (3-6). This may resulted from a sudden increase in oro- and hypopharyngeal pressure by instant closure of the velopharynx and anterior oropharynx. The perforation site suggest that the pathophysiology of this case may be different from that of esophageal perforation in Boerhaave's syndrome that is thought to be the result of a sudden rise in internal esophageal pressure produced during vomiting, as a result of neuromuscular incoordination causing failure of the cricopharyngeus muscle to relax.
Esophageal rupture often carries with a high morbidity and mortality, hence, early recognition is important. Late diagnosis, more than 24 hr after perforation, is associated with increased morbidity and mortality (1, 7, 8). Early diagnosis is often difficult and requires a high index of suspicion especially in patients with atypical presentation. A classical triad of constitutes Boerhaave's syndrome: forceful vomiting, chest pain, and subcutaneous emphysema. Pain is the most common symptom and is usually localized to the site of the perforation. In cervical perforations, neck pain may be accompanied by tenderness of the sternomastoid muscle (9). Surgical emphysema of the neck is also frequent after cervical perforations and commonly detected with plan X-ray or CT examination. The symptoms and signs seem to be presented earlier and more typically in the perforations of the pharynx or cervical esophagus than those of classic Boerhaave's syndrome. Respiratory or intrathoracic complications are uncommon in the pharyngeal or cervical esophageal perforation, occurring in approximately 10 percent of patients, compared with over 50 percent of patients with thoracic esophageal perforation (10). A swallow study with water-soluble contrast medium confirms the diagnosis and defines the exact site. In the present case, the perforation site was confirmed by both gastrografin swallow and CT examinations.
The management of spontaneous esophageal perforation is controversial and early surgical intervention is preferred in most cases of thoracic esophageal rupture (7, 8). The management depends upon the time of presentation, site of rupture and etiology. Most series of spontaneous pharyngeal or esophageal perforation were conservatively managed and cured without significant morbidity (3-6). Conservative management can be considered in patients with well-contained leak and no significant complications and include broad spectrum antibiotics and enteral/parenteral feeding (7, 10). Patients with a large, non-contained perforation and patients showing signs of shock or sepsis should be proper surgical intervention. Surgery consists of drainage with or without repair, esophageal diversion, or esophagectomy (7). In pharyngeal or cervical esophageal perforations, simple drainage of the paracervical space with or without primary repair, is commonly successful without significant morbidity and mortality (3-6, 10).
In conclusion, a rare spontaneous pharyngeal rupture can occur in a healthy patient after forceful vomiting. This case is unique as the tear site, involving the oropharynx and upper hypopharynx, differing from those of prior reports (3-6, 10). With clinical suspicion, initial examination of CT and contrast swallow studies should be performed as early as possible. The small uncomplicated pharyngeal rupture may resolve without surgical intervention.