125I Seed Permanent Implantation as a Palliative Treatment for Stage III and IV Hypopharyngeal Carcinoma
Article information
Abstract
Objectives.
The aim of this study was to investigate the feasibility and safety of percutaneous 125I seed permanent implantation for advanced hypopharyngeal carcinoma from toxicity, tumor response, and short-term outcome.
Methods.
125I seeds implant procedures were performed under computed tomography for 34 patients with advanced hypopharyngeal carcinoma. We observed the local control rate, overall survival, and acute or late toxicity rate.
Results.
In the 34 patients (stage III, n=6; stage IV, n=28), the sites of origin were pyriform sinus (n=29) and postcricoid area (n=5). All patients also received one to four cycles of chemotherapy after seed implantation. The post-plan showed that the actuarial D90 of 125I seeds ranged from 90 to 158 Gy (median, 127 Gy). The mean follow-up was 12.3 months (range, 3.4 to 43.2 months). The local control was 2.1–31.0 months with a median of 17.7 months (95% confidence interval [CI], 13.4 to 22.0 months). The 1-, 2-, and 3-year local controls were 65.3%, 28.6%, and 9.5% respectively. Twelve patients (35%) died of local recurrence, fourteen patients (41%) died of distant metastases, and three patients (9%) died of recurrence and metastases at the same time. Five patients (15%) still survived to follow-up. At the time of analysis, the median survival time was 12.5 months (95% CI, 9.5 to 15.4 months). The 1-, 2-, and 3-year overall survival rates were 55.2%, 20.3%, and 10.9%, respectively. Five patients (15%) experienced grade 3 toxic events and nine patients (26%) have experienced grade 2 toxic events.
Conclusion.
This review shows relatively low toxicity for interstitial 125I seed implantation in the patients with advanced stage hypopharyngeal cancer. The high local control results suggest that 125I seed brachytherapy implant as a salvage or palliative treatment for advanced hypopharyngeal carcinoma merit further investigation.
INTRODUCTION
Hypopharynx is the area of the pharynx that lies below the oropharynx, and it is visually inaccessible by routine office examination. Hypopharyngeal cancers are usually aggressive in behavior, they grow in a region of abundant lymphatic drainage, they do not produce specific early symptoms or signs, and usually occur in people who are nutritionally depleted and immunologically compromised. It is not surprising, then, that the survival rates for these cancers are poor [1].
The management of malignant neoplasms of hypopharynx remains difficult despite recent advances in surgical techniques, as well as multidisciplinary treatment programs [2,3]. Regardless of the type of therapy employed, high recurrence rates, and poor survival, significant alterations in speech and swallowing functions are common experience for patients with malignancies in this anatomic site.
Published studies describe the use of permanent implantation of 125I seeds for the treatment of head and neck malignancies. This novel technique ensures protracted cell killing over a period of several months through targeted delivery of high-dose radiation. The advantages of this technique are as follows: (1) it is minimally invasive, (2) dose distribution can be accurately predicted, (3) continuous irradiation increases the likelihood of damaging malignant cells in a vulnerable phase of the cell cycle, and (4) the incidence rate of acute adverse effects is low [4-7].
In this study, we investigated the feasibility and safety of percutaneous 125I seed permanent implantation for advanced hypopharyngeal carcinoma from toxicity, tumor response, and short-term outcome.
MATERIALS AND METHODS
Patients and staging
At the tumor hospital of Yunnan Province in the period between October 2008 and January 2013 totally 34 previously untreated patients with squamous cell carcinoma of the hypopharynx were included in this study. This study was approved by the Ethics Committee of Kunming Medical University, and all patients gave their informed consent for use of their data. The patients were all males whose age ranged from 53 to 81 years. The patients were staged according to the 2002 American Joint Committee on Cancer staging system. A complete medical history and careful head and neck examination was performed for assessment. Staging was made with help of computed tomography (extent of disease at the primary site, status of lymph nodes in the neck, and evaluation for metastatic disease). All of the patients were presented with advanced stage of disease (stage III–IV) (Table 1). The sites of origin were pyriform sinus (n=29) and postcricoid area (n=5). At our institution, in principal, the choice of radical therapy is surgery, including partial pharyngolaryngectomy and total pharyngolaryngectomy, and neck lymph node metastasis should treated by neck dissection. But all the 34 patients were not considered suitable for radical surgery and neck dissection because of the systemic disease with multi-organ involvement or the patients refused to receive total pharyngolaryngectomy. We choose the 125I seed implantation as an alternative treatment modality. All patients were evaluated Karnofsky performance status scores before implantation and the scores are higher than or equal to 70. All the 34 patients have no major impairment of kidney, liver, or bone marrow function.
Before the implantation, we evaluated the history and physical condition of all the patients, hematological and chemical tests, and the patients underwent head and neck and chest computed tomography (CT) scanning with a 5-mm thickness one week before seed implantation.
125I seed implantation
A detailed CT-aided tumor-volume study was also performed for all the patients 1 week before seed implantation. We obtained transverse images of the targets at 5-mm intervals. The images were transferred to a computerized treatment planning system (Beijing Atom and High Technique Industries Inc., Beijing, China) to construct the implantation plan. The planning target volume (PTV) was calculated through computerized treatment planning system by the radiation oncologist. The PTV included the gross tumor volume with a 0.5–1 cm margin.
Seed implantation was performed in all the 34 patients under adequate local anesthesia in the operating room with especial protective devices. After determining the target volume and drawing the targets surface projection (Fig. 1), 18-gauge interstitial needles were inserted into the tumor and metastatic lymph node through the skin surface under CT guidance. Most of the 18-gauge needles were placed 1.0-cm distance from each other in a parallel array in the PTV. Precautions were taken to avoid puncturing the large blood vessels and neural structures and other important organs. The median number of needles is 14 (range, 5 to 42). After placing the needles, 125I seeds (Shanghai GMS Pharmaceutical Co. Ltd, Shanghai, China) were implanted into the tumor (Fig. 2). We pressed the pinpoint for at least 5 minutes after withdrawing the needles in order to reduce the bleeding of pinpoint. Administration of prophylactic appropriate antibiotics is necessary to prevent postoperative infection.
The actuarial median number of the implanted 125I seeds was 48 (range, 32 to 92). The specific activity of 125I seeds was 0.6 mCi/seed. The total activity of the implanted seeds ranged from 19.2 to 55.2 mCi (median, 28.8 mCi). The evaluation of post plan shown the actuarial D90 ranged from 90 to 200 Gy (median, 127.5 Gy) [8]. The seed implanted volume ranged from 27 to 190 cm3 (median, 79.5 cm3).
Tumor response was first evaluated at 4 weeks after implantation. Subsequent evaluations were performed at 2- to 3-month interval for the next 2 years and 6-month interval, thereafter. The disease status was assessed by physical examinations, liver function tests, and complete blood and platelet counts. Disease progression was determined by means of imaging studies, including CT scans and ultrasonography. The follow-up time was calculated from the date of seed implantation. The median follow-up period was 12.3 months (range 3.4 to 43.2 months). The complications were scored using the Radiation Therapy Oncology Group (RTOG)/European Organization for Research and Treatment of Cancer late radiation morbidity score. The survival time was calculated from the date of implantation to the last date of follow-up or date of death. In these calculations, deaths due to any reason were scored as events. Local control was defined as the lack of tumor progression either in or adjacent to the implanted volume. Tumor responses were assessed using CT and ultrasonography according to the World Health Organization criteria. The quality of life (QOL) of patients was evaluated by University of Washington QOL questionnaire (version 2, Chinese language version). Final composite score before and after treatment were compared by chi-square test. The overall local control and survival times were determined using the Kaplan-Meier method by using SPSS ver. 10.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Symptomatic response
CT scan found that tumor was significant reduced (complete remission [CR]+partial remission [PR]) in 34 cases, one month after the operation, accounting 100%. Tumor was significant reduced (CR+PR) in 33 cases, three months after the operation, accounting 97%. Tumor was significant reduced (CR+PR) in 32 cases, six months after the operation, accounting 94%. 125I seed permanent implantation in treating patients with advance hypopharyngeal, the patients’ pronunciation and swallowing function can be preserved, which is very important for the palliative treatment of advanced cancer is concerned. Laryngeal function preservation was possible in all patients with 125I seed permanent implantation. All patients’ hypopharyngeal ventilation was well. There was no patients received incision of tracheotomy during observation period. Secondly, 125I seed permanent implantation treatment improves the symptoms caused by huge local tumor, such as difficulty in breathing and swallowing, and to some extent relieve pain caused by malignant tumor.
Doses to targets and critical tissues
The total activity of the implanted seeds ranged from 19.2 to 55.2 mCi (median, 28.8 mCi). The evaluation of post plan shown the actuarial D90 ranged from 90 to 200 Gy (median, 127.5 Gy). The seed implanted volume ranged from 27 to 190 cm3 (median, 79.5 cm3). Because the selected patients are different in local invasion range of tumor, the size of the tumor, and some patients could not tolerate the full-dose radiotherapy, we gave different radiation doses for different patients. All doses to targets and critical organs were the summations of all treatment plans including 3-dimensional conformal radiotherapy and intensity-modulated radiotherapy (IMRT).
Follow-up time
The follow-up time was calculated from the date of seed implantation and the median follow-up time was 12.3 months (range, 3.4 to 43.2 months) for all patients.
Local control
The median local control was 17.7 months (95% confidence interval [CI], 13.4 to 22.0 months), and the 1-, 2-, and 3-year local controls were 65.3%, 28.6%, and 9.5%, respectively (Fig. 3).
Survival
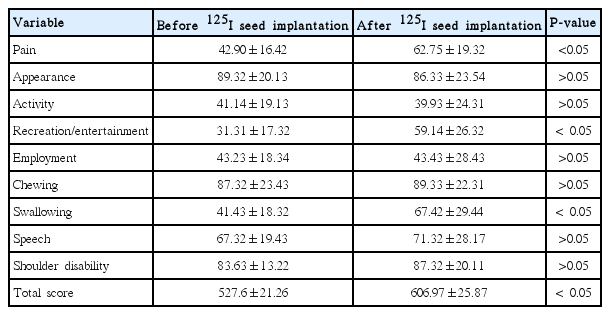
The median survival time was 12.5 months (95% CI, 9.5 to 15.4 months), and the 1-, 2-, and 3-year overall survival rates were 55.2%, 20.3%, and 10.9%, respectively. Of all patients, 12 patients (35%) died of local recurrence, 14 patients (41%) died of distant metastases, and 3 patients (9%) died of recurrence and metastases at the same time. Five patients (15%) still survive to the date of this analysis (Fig. 4). In terms of pain, recreation/entertainment, and swallowing, the QOL of patients was significant improved after 125I seed permanent implantation (P<0.05) (Table 2). While in term of speech, although there is some improvement, but there is no statistically significant (P>0.05). There is no significant improvement in other terms.
Function of larynx
Laryngeal function preservation was possible in all patients with 125I seed permanent implantation. Hypopharyngeal ventilation of all patients were well. There was no patients received incision of tracheotomy during observation period.
Acute toxicity
The most common complication was postoperative sore throat. Five patients (15%) suffered RTOG grade 3 complications. There are no RTOG grade 4 or 5 complications were observed. We did not observe postoperative nerve or blood vessel injury caused by radiation (Table 3, Figs. 5, 6).
DISCUSSION
It is the main objective to lengthen the survival time, preserve the phonation and swallowing functions, and promote organic recovery to treat hypopharyngeal carcinoma. However, in China, which is a developing country with a vast population as well as a limited medical resources, the management of advanced hypopharyngeal cancer is frequently facing financial or technical difficult.
The comprehensive treatment mainly comprised of surgery is the standard mode to treat hypopharyngeal cancer and the important guarantee to improve the tumor local control rate, and radiotherapy is the main treatment way for patients who cannot receive operative treatment. As for conventional radiotherapy, improving dose of radiation is the main way to improve the local control rate of tumors, but there is a tolerance dose of regular tissues. As a result, although traditional external beam radiation treatment could extend the survival period, its application should be limited to a certain extent because of its large radiation field, low tolerated dose of regular tissues. In order to retain the throat functions, many scholars use induction chemotherapy plus external beam radiotherapy, and Urba et al. [9] apply inducing chemotherapy and external beam radiotherapy in 22 cases of patients in the progressive stage, and it reveals that the overall 3-year survival rate is 64.0%. Lefebvre et al. [10] apply inducing chemotherapy and external beam radiotherapy in 116 cases of patients suffering hypopharyngeal carcinoma, which reveals that 3-year tumor local control rate is 49.7%, and five-year overall survival rate is 48.5%. Concurrent radiochemotherapy is an effective treatment way for squamous cell carcinoma in progressive stage and improves 10–20 survival rate or so compared with radiotherapy alone, and in particularly it could boost the survival rate prominently for unresectable cases and improve the retaining rate of throat functions. However, it has relatively significant toxic and side effects and some patients cannot endure [11]. Liu et al. [12] apply IMRT and combined chemotherapy at the same time for hypopharyngeal carcinoma patients of overall stage II–IV, and it reveals that 5-year tumor local control rate is 63.3%, disease free survival is 51.0%, and 63.0% patients have dysphagia above level 3. Therefore the patients and doctors fall into the dilemma of practicing giving-up therapy or not. Actually, in the face of serious complications, most patients requested that treatment must be halted.
When we meet some patients who cannot receive partial pharyngolaryngectomy and total pharyngolaryngectomy because of the systemic disease with multi-organ involvement, patients are difficult or impossible to accept such operation. Conventional radiotherapy is considered not satisfactory to advanced hypopharyngeal carcinoma. Seed-implant brachytherapy with image-guidance has been performed in head and neck malignant tumors treatment for some decades [13]. Radioactive seeds implantation brachytherapy in the internal radiotherapy catalogue has seen rapid development during recent years and provided new and effective treatment ways for patients that cannot receive operation, external beam radiotherapy, or recurrent cancer treatment. 125I has physical characteristics of low dosage rates, low photon energy (averagely 28 keV), and short effective penetration distance in the tissue (1.7 cm in soft tissue), so the doses to the surrounding normal tissues decrease very rapidly with distance, and are easily confined within the tumor target. Thus the image-guidance 125I seed permanent implantation which allows the application of a high radiation dose while avoiding severe adverse events can be applied to patients who are of advanced age with poor performance status or who have complications, thereby improving the prognosis of our patients [14].
Our hospital begins to attempt to apply 125I seed to implant into hypopharyngeal carcinoma patients of advanced stage who cannot endure operation and chemotherapy and mainly explore the feasibility and complications of the new therapeutic method. In this research, after radioactive seeds are implanted, the most ordinary severe acute radioactive damage is mainly dysphagia caused by radiation therapy-pharyngalgia, and we provide regular drug therapy and nutritional support. Then there are radioactive mucositis and dermatitis, of which the former is mainly level two, and we adopt regular treatment together with quinolone antibiotics and get effective control. Radioactive dermatitis is mainly of level one and gets recovery in 2–3 weeks, and skin pigmentation and fibrosis will appear in 3 months that do not need special treatment. However, acute radioactive damage will prolong the interval of supplementing seed or secondary seed and the total treatment therapy and affect treatment effects. The most common later radioactive damage is laryngostenosis, and if it is level 3, tracheotomy should be considered timely. The study shows a relatively high throat function retaining rate reaching 91% (31/34), 71% (23/34) patients get CR after implantation in two months, 26% (9/34) patients get PR after implantation, and 1 patient has no response after implantation. Within the follow-up period, the 1-, 2-, and 3-year local control rates were 65.3%, 28.6%, and 9.5%, respectively. The 1-, 2-, and 3-year overall survival rates were 55.2%, 20.3%, and 10.9%, respectively. The median survival period is 12.5 months.
Head and neck is the core part has many important functions closely related to daily life, such as speech, breathing, balance, and so on. Hypopharyngeal and tissue lesions and defect caused by treatment will lead to significant functional impairment and facial damage. It will seriously impacts patient’s psychological and social function, significantly reducing the quality of their life. We analyzed the selected patient’s quality of life after 125I seed permanent implantation treatment, the result shows that, despite the limited survival time delay, the overall quality of life can be improved. Comparing the functions between preoperative and postoperative, the most significant improvement are in pain and swallowing function, the speech function improved partially, thus the patients’ recreation is improved after the treatment, and it is also the most important aspects of quality of life after surgery. There is radiation-related pain after implantation. But because the pressure caused by advanced malignant tumor and the pain caused by tumor-induced infringement has been significantly alleviated, and therefore increased pain scores after treatment.
However, there is no control group in the study, it could not be ruled out that 125I seed tissue implantation has demonstrable advantages over conventional approaches. It is also observed that it is difficult for 125I seed tissue implantation to control distant metastasis of tumor, and it is necessary to further study if hypopharyngeal carcinoma of advanced stage can be treated together with combined chemotherapy so as to improve survival rates of patients.
In conclusion, 125I seed implantation is an effective salvage or palliative treatment method to treat the patients who cannot receive radical operation and has characteristics like high throat function retaining rates, minimal invasion, safety, convenience, high tumor local control rate, low complication occurrence rate, etc. It will be more comprehensive and correct to evaluate the efficacy and clinical significance of 125I seed tissue implantation to accumulate sample quantity continuously, conclude experiences, and strengthen long-term follow-up work.
HIGHLIGHTS
▪ 125I seed permanent implantation is a safe and convenient treatment with minimal invasiveness.
▪ It showed high local control rate and relatively acceptable complication.
▪ The quality of life of the patients improved significantly after the implantation.
Notes
No potential conflict of interest relevant to this article was reported.