INTRODUCTION
Obstructive sleep apnea (OSA) is a common disorder affecting at least 2% to 4% of adult population characterized by the collapse of the pharyngeal airway resulting in repeated episodes of airflow cessation, oxygen desaturation and sleep disruption [1]. According to the National Commission on Sleep Disorders, more than 40 million people in the United States are affected by sleep-disordered breathing until; in spite of these epidemiological data, until the year 2000 it was estimated that up to 93% of females and 82% of males with moderate-severe OSA remained undiagnosed and untreated [2,3]. Clinically, OSA is defined as the occurrence of daytime sleepiness, loud snoring, witnessed breathing interruptions, or awakenings due to gasping or choking in the presence of at least 5 obstructive respiratory events (apneas, hypopneas or respiratory effort related arousals) per hour of sleep.
It is well established that retropalatal region is the most common site of obstruction in patients with snoring and OSA syndrome [4]. Consequently, since the introduction of uvulopalatopharyngoplasty (UPPP) [5] many surgical techniques have been introduced aimed at creating scar tissue, inciting fibrosis and stiffening the palate. Among the proposed techniques [6,7], the reversible uvulopalatal flap (UPF) introduced by Powell et al. [8] also achieves the same results as the UPPP, but with less postoperative discomfort, less risk of developing velopalatal insufficiency, and fewer complaints of a thickened secretion or foreign body sensation.
The purpose of this study is to present the preliminary results of our experience in the modified cautery-assisted palatal stiffening operation (CAPSO) first introduced by Pang and Terris [9] in 2007 and renamed thereafter by the same authors, as anterior palatoplasty (AP).
Patients with mild-moderate sleep apnea were randomised to undergo either UPF or AP. Two specific outcomes were identified and addressed: 1) the efficacy of UPF and AP for mild-moderate OSA, 2) the morbidity associated with these two techniques.
MATERIALS AND METHODS
The present study is an unfounded, with no monetary support from any source, study and was approved by the Hospital Ethics and Research Committee (San Carlo Hospital, Rome).
Thirty-eight consecutive patients (25-male, 13-female) with mild-moderate OSA were prospectively enrolled into a randomised surgical protocol. Inclusion criteria were: 20 years of age or older, no evidence of morbid obesity (body mass index [BMI] <33), presence of mild-moderate OSA (apnea-hypopnea index [AHI] >5 and <30) as documented by polysomnography; tonsil size grades 1, 2 and 3, elongated uvula, minimal tongue base collapse as seen at the Müller manoeuvre, Fujita I (retropalatal obstruction), no prior surgical intervention for sleep apnea and no contraindications to surgery. Informed consent was given by each patient.
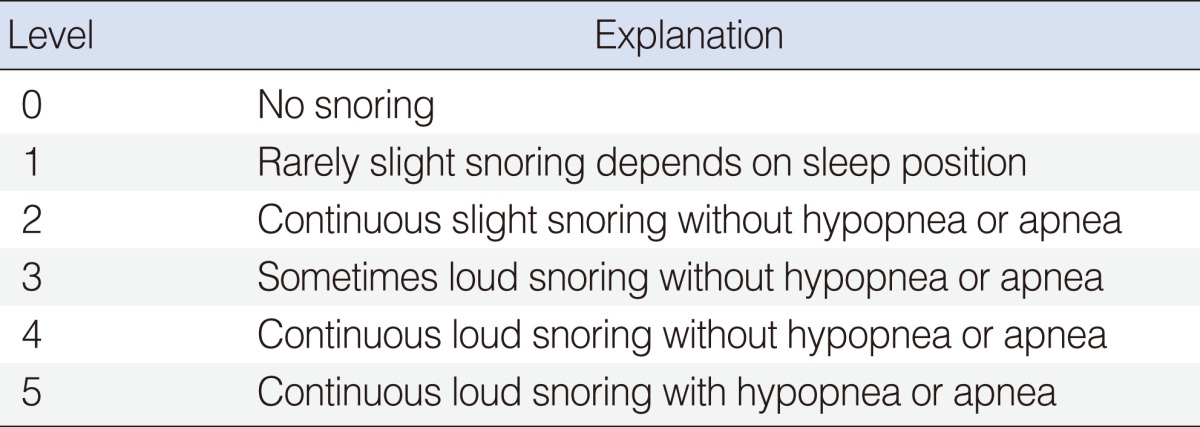
The parameters considered in this study were the evaluation of OSA severity and postoperative pain. OSA severity was evaluated analysing the subjective and objective assessment of snoring by: 1) patients' roommates completed snoring assessment questionnaire (SQ) (Table 1); 2) the evaluation of daytime sleepiness by the Epworth Sleepiness Scale (ESS) completed by patients before and two months after surgery and 3) the registration of retropalatal Müller grade according to a 5-point scale from 0 to 4 (Table 2). The patients also completed a visual analogue scale (VAS) for postoperative pain from day 1 to 14 after surgery.
The patients were evaluated during in and out visits scheduled on the first and third days, 1 and 2 weeks and 2 months postoperatively. The postoperative assessment included a complete head and neck examination, with emphasis on the endoscopic evaluation of the posterior nasal space, and the oropharyngeal area, soft palatal redundancy, uvula size and Müller manoeuvre.
Surgical success was measured primarily by satisfactory reduction in snoring, as reported by SQ of sleep partners completed before and two months after surgery (Table 3). Secondary outcomes measures included improvement in the Epworth scale scores, changes in the magnitude of pharyngeal collapse and palatal length, and postoperative pain intensity.
The polysomnography was repeated between 6 and 9 months after surgery and surgical response was determined by criteria proposed by Sher et al. [10] of a 50% reduction in the AHI and a postoperative AHI of less than 10.
Surgical technique
Uvulopalatal flap
UPF was performed as describe originally by Powell et al. [8] in general anaesthesia. The mucosa, submucosa with glands, and fat on the lingual surface of the uvula and soft palate were removed with scalpel. The uvular tip was amputated and bleeding was controlled by bipolar electrocoagulation. The uvula was reflected back toward the soft palate and fixed into its new position with multiple sutures of 3/0 Vicryl.
Anterior palatoplasty
This procedure was performed as describe by Pang and Terris [9], according the modification in which general anaesthesia is used instead of local anaesthesia. As first step an uvulectomy may be performed, followed by vertical cuts on either side of the uvula through both soft palatal arches. A horizontal rectangular strip of mucosa (40-50 mm in length and 7-10 mm in width) was thereafter removed from the soft palate 10 mm to the limit of soft palatal arches, down to the muscular layer. No less than 9 sutures were used to suture the horizontal stripped area with a Vicryl 3/0 round body-curved needle (Fig. 1).
In both surgical procedures a tonsillectomy was first performed if the patient had relatively large tonsils (tonsil size 2 and 3). Postoperative medications included antibiotic suspension for 7 days and acetaminophen as needed for pain relief.
Statistical analysis
The results were statistically evaluated by comparing mean values of each preoperative parameter (ESS, palatal collapse, palatal length and SQ) together with postoperative pain evaluation in the two surgical techniques groups using the unpaired t-test. A t-test was used also to determine if there was any difference between the 2 groups with respect to age, sex, BMI or OSA severity.
RESULTS
Thirty-four (98.4%) out of thirty-eight patients completed all pre- and postoperative protocol. No statistically significant differences were noted between the two groups with regards to any demographic or disease severity parameter (BMI, age, sex, AHI, ESS) used in this trial. Fifteen patients were randomised to AP, 19 to UPF.
In AP group on 15 patients 3 had prior surgical intervention in young age, in 10 we performed tonsillectomy (six patients with tonsils size grades 2 and four with grades 3) and in 2 patients with tonsil size grades 1 we didn't performed tonsillectomy.
In UPF group on 19 patients 4 had prior surgical intervention in young age, in 10 we performed tonsillectomy (five patients with tonsils size grades 2 and five with grades 3) and in 5 patients with tonsil size grades 1 we didn't performed tonsillectomy.
The mean operative time was 35±15 minutes for AP patients and 37±18 minutes for UPF patients. There were no complications in both groups; specifically, no patients with velopharyngeal incompetence, oronasal fistula or primary or secondary haemorrhage.
Anterior palatoplasty
This group patients had a mean age of 48.3±10.2 years, BMI at the time of surgery ranged from 25.2 to 28.2 (mean, 26.5±2.4) and there were no significant BMI changes after surgery. Preoperative mean of AHI was of 22±12.5; the ESS mean was preoperative 8.5±3.7 and postoperative 4.9±3.2 (P<0.001). Twelve (80%) out of 15 patients achieved a satisfactory reduction in the volume of snoring, as reported by the sleep partner SQ, 2 months postoperatively (Table 3). The collapse noted at Müller manoeuvre during upper airway examination improved from 2.7±1.0 on average to 1.1±0.9 (P<0.001). A representative postoperative picture is shown in Fig. 2. The polysomnography showed that AHI in 13 of the 15 patients (86%) improved from the mean of 22±12.5 to 8.6±6.8 (P<0.001) reaching a surgical response according the criteria established by Sher et al. [10].
Uvulopalatal flap
This group of patients had a mean age of 46.2±11.2 years, BMI at the time of surgery ranged from 24.8 to 28.4 (mean, 26.6±2.3) and there was no significant difference between pre- and postoperative BMI values. The mean AHI was 23±12.3 preoperatively, whereas the EES mean was preoperatively 8.1±3.5 and 5.2±3.2 postoperatively (P<0.001). Fourteen out of 19 patients (73.6%) achieved a satisfactory reduction in the volume of snoring, as reported by sleep partner SQ 2 months postoperatively (Table 3). The collapse noted at Müller manoeuvre improved from 2.8±1.1 on average to 1.8±1.1 (P<0.05). A representative postoperative picture is shown in Fig. 3. The polysomnography showed that 16 of the 19 patients (84%) achieved a surgical response when applying criteria established by Sher et al. [10], the AHI mean decrease from 23±12.3 to 9.6±7.8 (P< 0.001).
Pain assessment
Variation of pain with VAS was determined at postoperative follow-up. Postoperative oedema was present in all cases. Duration of oedema varied from 3 to 14 days (mean, 8 days). Complaints of pain (beginning in the early postoperative period, peaking on the 2nd day, and lasting from 3rd to 14th day) and difficulty in swallowing were evaluated all along this period of time. None of the patients needed analgesics or re-hospitalization for intractable pain. The mean duration of pain was 10.8 days for UPF patients and 7.1 days for AP patients. This difference was statistically significant (P<0.05). The mean pain score was 6.8 for UPF patients and 5.1 for AP patients for the first 3 days. VASs for pain are shown in Fig. 4.
DISCUSSION
Continuous positive airway pressure (CPAP) is the treatment of choice for adult patients with mild-moderate OSA. However, adherence to CPAP is insufficient in 17% to 54% of patients [11]. Therefore, over the last three decades various operation have been developed at the level of palate aimed at improving airway patency by stiffening the pharyngeal wall. Palatal surgery is now the largest established surgical approach to snoring and mild-moderate OSA [12].
The UPF procedure described by Powell et al. [8] provides the same results as the UPPP introduced in 1985 [5] as already demonstrated in several studies but with less postoperative patients' discomfort. Pang and Terris [9] in 2007 introduced AP as alternative surgical procedure to stiffen the palate surface.
According to the literature, short-term improvements occur in 88% of UPF treated patients [13]. In this preliminary study the AP results were comparable to UPF subjective results: in fact the ESS after AP improved from a preoperative value 8.5±3.7 to a postoperative mean of 4.9±3.2 (P<0.001). In a similar way, the ESS values after UPF improved from a preoperative value of 8.1±3.5 to 5.2±3.2 postoperatively (P<0.001).
The results of satisfactory reduction in the volume of snoring, as reported by sleep partner SQ 2 months postoperatively, were also similar in both surgical procedures. In fact partners' SQ reached 0 level in 12 (80%) of AP cases. When compared with UPF postoperative partners' SQ-improved until level 0, in fourteen (73.6%) cases-no significant difference was found between the two groups. And compared to a similar response at polysomnographic data of the two surgical techniques the real superior efficacy came from the data of palatal collapse during Müller manoeuvre and pain assessment.
We reported a statistically significant difference of the collapse noted at Müller manoeuvre that improved from 2.7±1.0 on average, to 1.1±0.9 (P<0.001) after AP and with a lesser extent, (from 2.8±1.1 on average to 1.8±1.1; P<0.05), after UPF probably because UPF although produced with the reposition and stabilization of uvula on the soft palate the wide opening of retropalatal airway space, therefore narrowing the lateral distance between the tonsillar pillars. Moreover during the postoperative objective examination (Figs. 2, 3) we noted a major anterior rotation of the palatal wall in AP than in UPF that also showed a higher thickness and alteration of normal anatomy (absence of uvula).
The pain was significantly more intense and prolonged in the UPF group compared with the AP group. The mean duration of pain was 10.8 days for UPF patients and 7.1 days for AP patients. This difference was statistically significant (P<0.05). The mean pain score in the first 3 days, was 6.8 in UPF patients and 5.1 in AP patients.
The subjective and objective improvements evidenced in this study may suggest how AP is far superior to other techniques aimed at creating a palatal fibrotic scar confirming the advantages already described by Pang et al. [14].
In short term, the effectiveness of both UPF and AP procedures was very high. Post operative pain was mostly seen in UPF lasting longer than in AP cases. In the light of these results and in spite of similar success rates we can suggest AP procedure as more practical and comfortable when compared to UPF.