INTRODUCTION
Curative doses of radiation therapy for laryngeal cancer may cause variable degrees of laryngeal edema. Although this edema usually subsides within a month or two, persistence of significant edema of larynx makes careful inspection and evaluation of the larynx difficult (1). Moreover, it may have impacts on functions such as breathing, swallowing, speech and voice (2). Conservative management with voice rest, discontinuation of alcohol and cigarettes, a course of antibiotics and steroid may be attempted (3, 4). However, progressive and unresponsive edema may lead to airway compromise or aspiration pneumonia requiring tracheotomy.
We present four patients with persistent dyspnea due to arytenoid edema after radiation therapy for laryngeal and hypopharyngeal cancer, who underwent partial resection of the arytenoids mucosa using the CO2 laser. The procedure was performed when the patient showed stridor despite of medical treatment. Such a procedure for postradiation edema has not been reported in the literature and the procedures were successful in all the four cases.
CASE REPORTS
Case 1
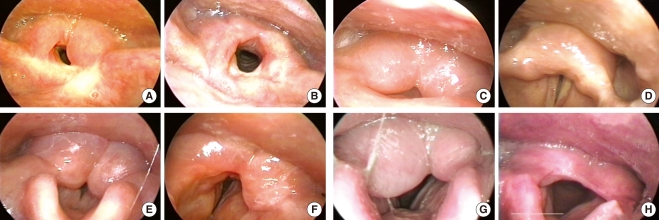
A 66-year-old male patient diagnosed as supraglottic cancer (T2N0M0), underwent laser supraglottic laryngectomy with concomitant tracheotomy and bilateral selective neck dissection. Pathologic result revealed cervical lymph node metastasis and the patient underwent 8-weeks of adjuvant radiation therapy. Total dose delivered was 5,040 cGy by 180 cGy per fractions, one daily fraction five times per week. Two months after the radiotherapy, dyspnea, dysphagia and aspiration due to edema of the arytenoid was detected. Oral steroid and antibiotics was given for 1 month but showed no improvement with persistent stridor (Fig. 1A). Three months after the radiotherapy, the patient underwent bilateral partial resection of the arytenoid mucosa via suspension microlaryngoscopy using the CO2 laser. The procedure was conducted under general endotracheal anesthesia using an aluminum-wrapped rubber tube. The arytenoid was exposed by anterior displacement of the tube with the suspension laryngoscope. The extent of the edema was evaluated through the operating microscope (OPMI Vario, Carl Zeiss, Oberkochen, Germany) revealing no evidence of any remnant or recurrent cancer. Using the CO2 laser (C33, Sharplan, Tel Aviv, Israel) at 2-3 watts superpulsed continuous power with focused spot size of 270 µm, we primarily delineated the medial portion of the edematous mucosa (Fig. 2A). The mucosa was grasped with a microlaryngeal cup forcep with medial traction and was separated from the arytenoid as en-bloc resection using the CO2 laser (Fig. 2B). Vocal cord, trachea and soft tissues of the posterior commissure were protected with saline-soaked cotton strips. Serous materials from the resection surface was sucked out to resolve the edema and bleeding was controlled using the suction Bovie. The arytenoid cartilage was not exposed to prevent postoperative chondritis, necrosis and fixation. Inferior portion of the arytenoid was also protected not to give any injury to the cricoarytenoid joint. Although there was no disturbance of the surgical view due to bleeding we made a thorough evaluation for any possible bleeding focus, since postoperative bleeding could lead to life-threatening condition. Biopsy of the edematous portion of the arytenoid revealed no evidence of any remnant or recurrent cancer. Tracheotomy was not performed as we determined it to be unnecessary. Dyspnea dramatically subsided several days after the surgery, however dysphagia and discomfort remained for several months until it eventually improved. The patient showed no dyspnea nor any evidence of recurrence up to 51 months after the surgery (Fig. 1B).
Case 2
A 74-year-old male patient diagnosed as supraglottic cancer (T2N0M0) underwent 10-weeks of radiation therapy at the dose of 6,840 cGy. Three weeks after the treatment the patient developed dyspnea and the laryngeal endoscope showed edema of both arytenoids drawn into the vocal cord on inhalation (Fig. 1C). Medical treatment was unsuccessful and the patient underwent partial resection of the arytenoid mucosa 16 months after the radiation therapy. The procedure was conducted under general anesthesia without tracheotomy. The patient showed no dyspnea within a week, and is under follow-up with no evidence of recurrence, 21 months after the surgery (Fig. 1D).
Case 3
A 78-year-old female patient diagnosed as glottic cancer (T1b-N0M0) underwent 8-weeks of radiation therapy at the dose of 6,840 cGy. Aspiration and dyspnea developed 1 month after the radiation therapy and severe edema of both arytenoids was identified (Fig. 1E). Medical treatment was unsuccessful. Partial resection of the arytenoid mucosa was conducted 8 months after. Since the edema was too severe, tracheotomy under local anesthesia was performed before the procedure to prevent aspiration from postoperative hemorrhage or decreased movement of the vocal cord. Biopsy from the removed tissues revealed no evidence of any remnant or recurrent disease. Decannulation of the tracheotomy tube had to be delayed to 6 months after the surgery due to poor movement of both the vocal cords which eventually improved to normal function. The patient showed no signs of airway compromise nor any phonation disorder up to 17 months after the surgery (Fig. 1F).
Case 4
A 67-year-old male patient diagnosed as hypopharyngeal cancer (T1N3M0) underwent 5-weeks of radiation therapy at the dose of 6,120 cGy following modified radical neck dissection. Dyspnea developed 2 month after the radiation therapy and severe edema of both arytenoids was identified (Fig. 1G). Medical treatment was unsuccessful and partial resection of the arytenoid mucosa was performed 4 months after the radiation therapy. Tracheotomy under general anesthesia was conducted before the procedure. Decannulation was conducted 30 days after the surgery. The patient showed no signs of airway compromise or recurrence up to 33 months after the surgery (Fig. 1H).
DISCUSSION
Arytenoid edema following radiation therapy results from blocked vascular and lymphatic outflow, in addition to increased vascular permeability (1). Fibrotic change from radiation leads to the blockage of these vessels more frequently in the supraglottic lesion where the capillary lymphatics are more larger and deeper than those of the vocal cord (3). It has been reported that 20.9% (3) to 59% (5) of patients presented with postradiation laryngeal edema.
Considering that arytenoid cartilage is articulated on the rostral surface of the cricoid cartilage which is the narrowest part of the upper airway, maximal airway enlargement could be achieved by removing the intraluminal portion of the arytenoids (6). Therefore, partial resection of the medial edematous portion occupying the lumen could be a effective procedure in case of arytenoid edema causing airway compromise. Resection of postradiation arytenoid edema using the transoral CO2 laser has never been reported in the English literature.
Although it may seem to be a simple surgical procedure, excessive laser injury to the arytenoid cartilage especially to the inferior portion may produce cricoarytenoid joint injury with subsequent fusion of the arytenoid to the cricoid, or even further medialization of the arytenoid secondary to soft tissue scar (7). We experienced one case of temporary vocal cord fixation requiring delay of decannulation. However the vocal cord showed normal movement in 6 months. We assume that mucosal inflammation due to the laser injury extending to the cricoarytenoid joint caused the fixation and since there was no permanent injury to the joint the fixation was reversible. Excessive laser injury to the cartilage can also cause mucosal stenosis, stricture and perichondritis and thus should be avoided during the procedure.
Major advantages of resection of the arytenoid edema with CO2 laser is as the followings. 1) Biopsy of suspicious lesions can be conducted simultaneously. As it has been well reported, persistence and progression of arytenoid edema after radiation therapy may accompany residual or recurrent cancer (1, 3, 8). Thus, inspection for such findings would be mandatory and could be followed by salvage laser surgery if malignancy is confirmed during the procedure. 2) Recurrence of edema is relatively rare compared to conservative medical treatment since the procedure is surgical debulking leading to airway enlargement. 3) Permanent tracheostomy can be avoided leading to early recovery and lesser complications. 4) Inspection of the larynx at the out-patient department becomes easier with enlarged airway space. 5) The procedure can be repeated in cases of insufficient airway enlargement.
Resection of the arytenoid edema after radiation therapy using transoral CO2 laser is an effective procedure to enlarge the airway. The surgical technique could be helpful for head and neck surgeons to manage airway problems after radiation therapy.