INTRODUCTION
A perilymph fistula (PLF) is defined as an abnormal communication between the inner ear fluids and the middle ear space (1). There are a variety of causes of a PLF including iatrogenic injury, idiopathic, trauma, and congenital anomalies. Among these, trauma is the third most common cause of PLFs followed by iatrogenic and idiopathic causes (2). Trauma, such as head trauma, barotrauma and acoustic trauma can cause oval or round window membrane rupture by direct or indirect force to the windows, or abrupt changes of cerebrospinal fluid pressure and/or middle ear pressure.
The primary manifestations of traumatic PLFs are usually sensorineural hearing loss and dizziness after trauma (2). In addition, tinnitus, ear fullness or hyperacusis can be accompanied. Hearing loss is usually sudden or progressive after the trauma. Sometimes, it may take two to three days after the trauma to notice hearing loss. Dizziness usually manifests as severe vertigo, disequilibrium or positional dizziness following the trauma. The severity of hearing loss and dizziness might be related with the severity of trauma. For example, if total deafness and acute vertigo with spontaneous nystagmus are developed by a PLF immediately after head trauma, this means that total homeostatic disruption of inner ear has happened and the prognosis will be poor. However, if hearing loss is mild or moderate and dizziness is positional, this means that the PLF is not so severe that the symptoms can be recovered with optimal management.
Treatment of traumatic PLF remains controversial. Because there are no definite diagnostic criteria for the PLF, not a few of patients suspected of having a PLF have been treated by conservative methods rather than surgical exploration; surgery is generally performed in patients with recurrent vertigo or progression of symptoms (1, 3, 4). In addition, even for patients strongly suspected of having a PLF, surgery could be delayed too long that accurate surgical outcomes could not be established (3).
There have been several reports regarding PLFs (5-7), however, these reports included many different causes in addition to traumatic causes. Glasscock et al. (2) reported 68 surgical cases of traumatic origin. Among them, only nine cases (13%) had a definite PLF identified at surgery. Hearing was improved in one case out of the nine that underwent surgical repair five days after trauma. They reported that dizziness could be improved by surgical repair, but hearing improvement was not common. However, they didn't divide patients according to the severity of injury and time interval between surgical repair and trauma.
The author's hypothesis is that prognosis of traumatic PLF is different according to the type and severity of injury. If the head trauma is so severe that total deafness and unilateral vestibular loss were induced, the prognosis will be poor regardless of management. However, if the hearing loss and dizziness is mild, usually induced by mild trauma such as barotrauma, the prognosis will be favorable once the fistula is repaired as soon as possible to prevent further leakage. In addition, once the oval and round windows are torn by the pressure, it will be difficult to heal spontaneously. Because both windows are continuously moving during sound conduction. Also, if the patients try Valsalva maneuver or nasal blowing to clear their symptoms, these make spontaneous healing more difficult. Therefore, the surgical repair for PLFs is more reliable method than conservative method. In addition, the earlier the fistula repair is done, the better chances would be regarding hearing outcomes and dizziness control.
The purpose of this study is to assess the outcomes of hearing after surgery in suspicious barotraumatic PLF according to the time interval between the trauma and the surgical repair. We try to emphasize the patient selection and timing of surgical repair for better hearing outcomes.
MATERIALS AND METHODS
The medical records of nine patients that underwent exploratory tympanotomy from January 2005 through December 2010, with the clinical impression of a barotraumatic PLF, were reviewed. PLFs were suspected with a history of sudden or progressive sensorineural hearing loss and positional dizziness following barotrauma. Sometimes, a 'popping' sound was heard at the moment of a traumatic event and tinnitus and ear fullness were followed. Types of barotrauma includes internal barotrauma such as heavy lifting, nasal blowing and straining and external minor trauma such as slap injury and other minor blunt trauma. Severe traumatic head injury to cause the temporal bone fracture and pneumolabyrinth were not included. Because these type of injury usually cause permanent deafness and total vestibular loss immediately after head trauma. The patients with inner ear anomalies, iatrogenic PLFs following ear surgery were also excluded.
Preoperatively, the types of trauma, otological symptoms and signs, time interval between the traumatic event and surgery were evaluated. In addition, the operative findings, postoperative changes in symptoms including hearing levels and dizziness, were analyzed. The hearing outcomes according to the time interval after surgery were compared.
In all cases of a suspected barotraumatic PLF, surgical exploration was performed as soon as possible by one otolaryngologist. Local anesthesia was preferred but general anesthesia was provided to uncooperative patients. After the tympanomeatal flap was elevated, the oval window (OW) and round window (RW) were fully exposed. Both window areas were carefully inspected for a possible perilymph fistulous site. Whether or not evidence of PLF was found, both windows were covered with soft tissue harvested from an endaural incision site. Then, fibrin glue was applied and the tympanomeatal flap was repositioned (Fig. 1).
After the surgery, the patients were instructed not to participate in activities that could raise the intracranial or intraabdominal pressure for a couple of days. Prophylactic antibiotics were used for a week. The patients returned to the outpatient clinic at one week and three weeks after hospital discharge for evaluation of symptoms. Two months after the surgery, an audiometry was performed. The hearing outcome was analyzed by pure tone audiometry at two months after surgery. Pure tone averages in four-frequencies (0.5, 1, 2, and 4 kHz) were used to compare.
RESULTS
Subjects
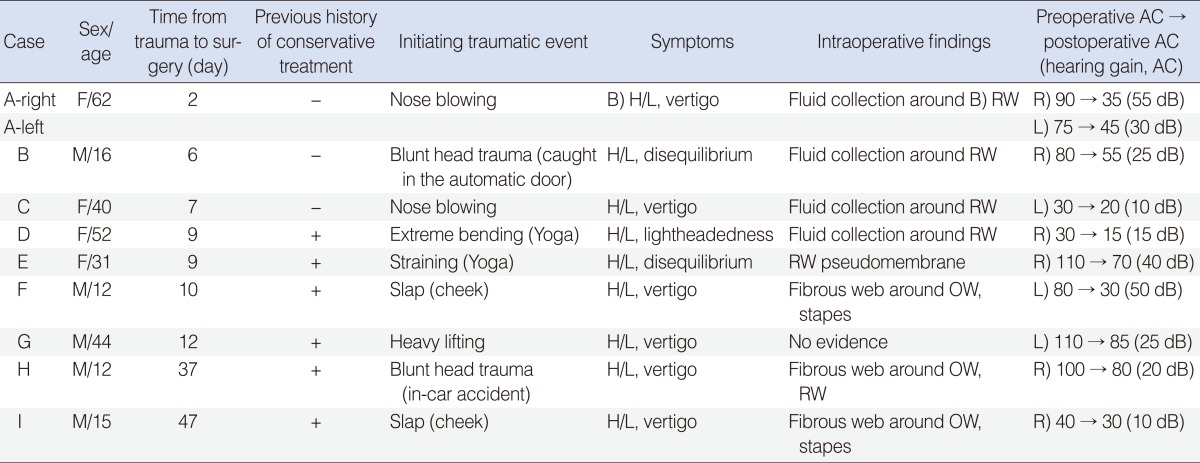
Ten operations were performed on 9 patients for suspected barotraumatic PLFs. One patient underwent surgical exploration in both ears, because bilateral hearing loss developed after severe nasal blowing. There were 4 males and 5 females aged from 12 to 62 years old, with a mean age of 32.
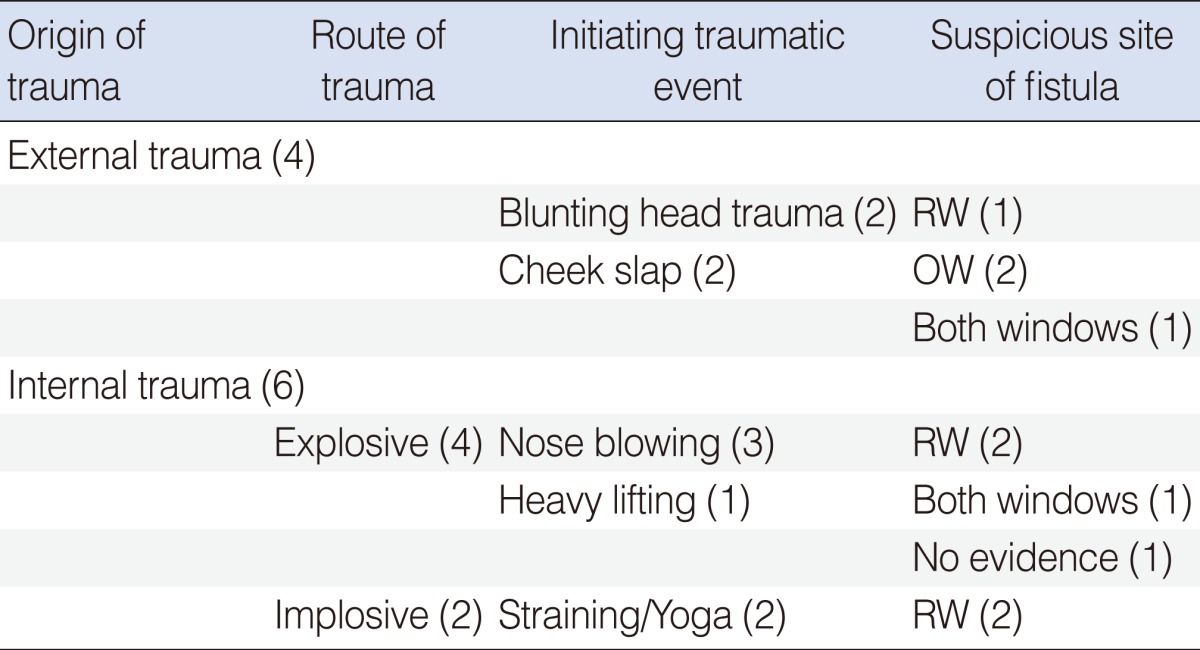
Types of antecedent trauma
Type of trauma was referred to Glasscock's classification of traumatic PLF (2). Traumatic PLF can be categorized into external trauma (blunt or penetrating head trauma, acoustic trauma) and internal trauma (barotrauma and trauma due to physical exertion). Among the 9 patients, 4 patients were classified as the external trauma (2 blunt head trauma from minor car accidents, 2 cheek slap injury) and 5 patients (6 cases) had internal trauma. Among 5 internal traumas, 3 patients had history of physical exertion such as heavy lifting (1 case) and nose blowing (3 cases) which could cause PLF by explosive route. Two patients gave history of an intense Valsalva maneuver during Yoga that might cause PLF by implosive route (Table 1).
Symptoms and signs
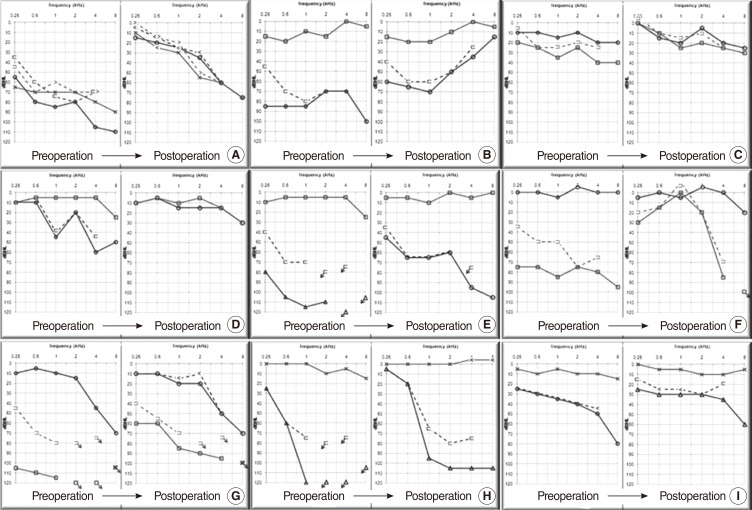
All patients had sudden or progressive hearing loss and dizziness. The hearing loss and dizziness developed immediately after the trauma in 7 patients. The others noticed their hearing loss and dizziness a few days after the trauma. Six patients had severe to profound sensorineural hearing loss and 3 patients showed serviceable hearing before the operation (Fig. 2). But, there were no patients with total deafness. The audiograms had a down sloping configuration. Air bone gap, especially in low frequency (250, 500, and 1,000 Hz), was found in 5 cases (Fig. 2A, B, E-G).
Regarding vestibular symptoms, six out of 9 patients complained of recurrent vertigo related to positional changes and aural pressure. The other 3 patients had disequilibrium and lightheadedness related to the traumatic events. Spontaneous horizontal nystagmus to ipsilateral side was observed only in 1 patient. However, there was no sign of permanent vestibular loss such as spontaneous nystagmus to contralateral side and head thrust sign.
On the endoscopic examination of the tympanic membrane, 1 patient showed hyperemia and blebs on both tympanic membranes. The other 8 patients showed normal tympanic membrane.
Three patients visited to the hospital without any previous treatment and underwent surgical exploration immediately due to a suspected PLF. However, 6 patients received conservative treatment including bed-rest and oral corticosteroids for 4 to 15 days at other hospitals and were transferred to this hospital without any improvement in their hearing. Surgical exploration was also done to these patients immediately after referral.
Intraoperative findings
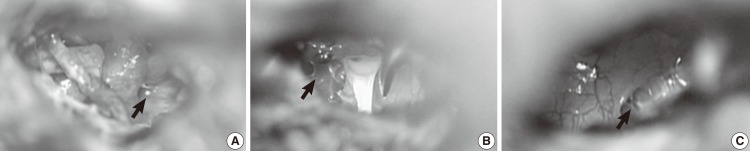
During surgery, the OW and RW were exposed and carefully searched for a possible fistulous site. Out of 10 ears, the RW was suspected as a fistula site in 6 cases, the OW in 2 cases and both windows in 1 case. In 1 case, there was no evidence of PLF. In 6 cases with a suspected RW fistula, fluid or pus collections were found in 5 cases (Fig. 3A), and the RW pseudomembrane was bulging in 1 case. In a suspected OW fistula, mesh like fibrous material was found around the stapes (we call it 'fibrous web') in 3 cases (Fig. 3B). In both windows suspected, fibrous web was found around RW and OW (Fig. 3B, C). In every patient, both windows were obliterated with soft tissue and fibrin glue, whether suspected fistulous sites were found or not.
Surgical outcomes and related factors
After the surgical repair, changes in symptoms were evaluated by the report of subjective dizziness and audiometry.
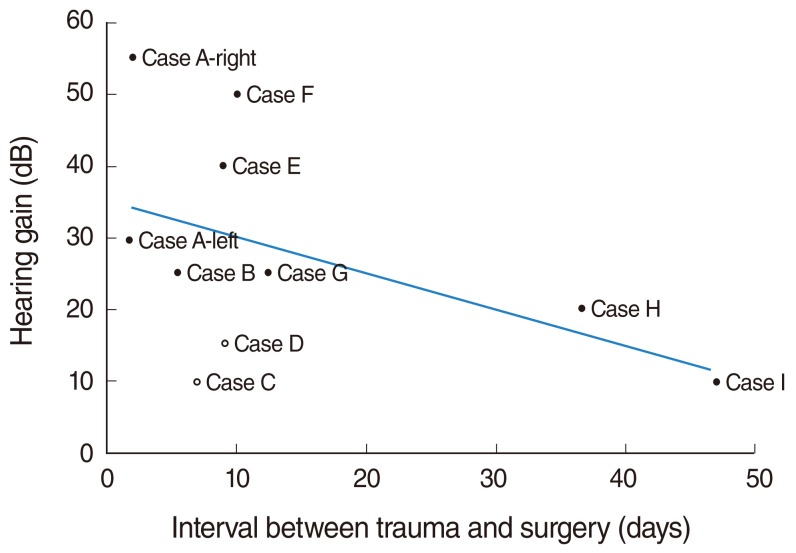
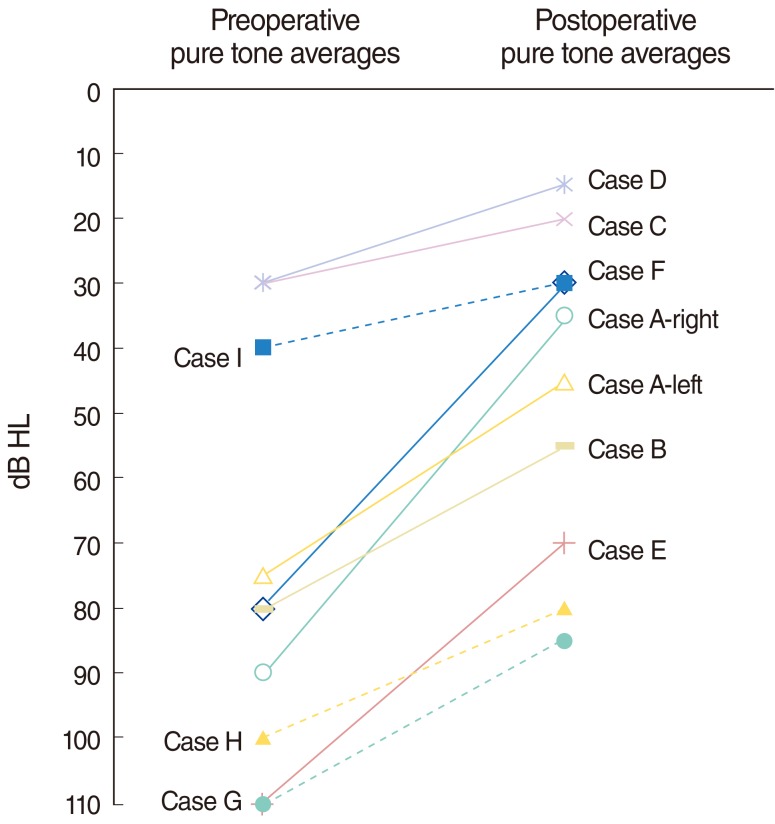
In all patients, dizziness resolved immediately after the operation. Regarding the hearing outcomes, every patient has improved significantly their hearing (>10 dB). The mean hearing gain was 27.0┬▒14.9 dB (range, 10 to 55 dB) in pure tone averages and 27.4┬▒32.6% (range, 0 to 92%) in speech discrimination score at 2 months after the operation. Serviceable hearing (pure tone averages in 4 frequencies Ōēż40 dB) was achieved in 5 out of 10 cases (50%) (Fig. 2A, C, D, F, I). In addition, hearing outcomes were analyzed according to the time interval between the trauma and the surgical repair (2, 6, 7, 9, 10, 12, 37, 47 days) (Fig. 4). If surgery was done before 10 days after trauma, serviceable hearing was achieved in 4 out of 7 (57.1%) compared to 1 out of 3 (33.3%) after 10 days after trauma (Fig. 5).
DISCUSSION
There have been few studies that considerable hearing gain had been achieved after surgical repair of PLFs. Also, it has been thought to be very difficult to predict the hearing outcomes in patients with suspected PLFs. Black et al. (8) and Goto et al. (5) reported that the patients showed improved hearing in only 17% and 9%, respectively. Compared with previous results of hearing improvement after surgery, the results found in our cases were significantly better. In this study, all 9 patients (10 cases) that underwent urgent surgery obtained a 10 to 55 dB improvement in hearing after the surgery. The mean hearing gain was 27.0┬▒14.9 dB and postoperative hearing improved to serviceable level (Ōēż40 dB) in 5 out of 10 cases. In case of Black et al. (8), the 6 weeks of conservative management was done before the surgery in all patients without progressive hearing loss. It could mean that satisfactory result in hearing might not be expected despite of enough duration of conservative treatment. And in case of Goto et al. (5), the duration of symptom was more than 1 month. So, we focused on the timing of surgical intervention.
When the surgical exploration was performed as early as less than 10 days after the trauma, serviceable hearing (Ōēż40 dB) was obtained in 4 out of 7 cases (57.1%) compared to 1 out of 3 cases (33.3%) which were repaired after 10 days. Better result for hearing improvement in this study might be due to patient's selection and timing of surgical intervention.
The diagnosis of traumatic PLF is mostly based on the clinical findings, including the history, physical examination and audiogram. Unfortunately, because there is no definite diagnostic test for PLFs, careful history taking is needed. Important part of patient's history is antecedent trauma and symptoms. According to Glasscock's classification, traumatic etiologies of PLFs can be categorized into head trauma, barotrauma, acoustic trauma and trauma caused by physical exertion (2). Looking at these etiologies in more detail, it can be divided into internal and external trauma. External trauma is that the origin of trauma exists outside of human body, literally. So, blunt or penetrating head trauma and acoustic trauma would be the external trauma. On the other hand, barotrauma and trauma caused by physical exertion would be the internal trauma. Among the internal trauma, the PLFs caused by physical exertion such as weight lifting, coughing and sneezing are suspected in mechanisms that increased cerebrospinal fluid pressure transmitted to the labyrinth via the cochlear aqueduct or internal auditory canal (explosive route). Whereas, the mechanisms of PLFs in barotrauma are suspected that sudden or severe changes in middle ear pressure via the Eustachian tube are theorized to direct force internally toward the inner ear, causing rupture of the OW or RW membranes (implosive route). So, these kinds of trauma followed by sudden or progressive sensorineural hearing loss and dizziness should raise concern about a barotraumatic PLF (2, 3).
In our series, the audiometric configuration showed descending types (8 cases). This means that the basal turn of the cochlea was more vulnerable to be damaged by a fistula because of the proximity to the OW or RW. In addition, the hearing recovery was better at low frequencies. In seven cases, an air-bone gap at low frequencies (250, 500, and 1,000 Hz) was found. These findings might reflect the third window effects associated with a PLF (6). After surgical repair, the air-bone gap of 250 Hz decreased to less than 20 dB (Fig. 2).
Dizziness associated with a PLF is characterized by positional vertigo and disequilibrium after trauma. However, there was spontaneous nystagmus of irritative type noted only in one case; this indicates that acute loss of semicircular canal function happens rarely. The dizziness might be caused by transient otolithic dysfunction or perilymph perturbation. After the surgical repair, all patients had resolution of the vestibular symptoms. This is consistent with previous studies that reported the vestibular outcomes to be better than the hearing results and the improvement rate for dizziness was more than 80% (7-9). Also, there was no sign of permanent vestibular loss including the head thrust sign or paralytic spontaneous nystagmus. We excluded the patients with severe external head trauma. Because if the head trauma is so severe that the cochlear and vestibular hair cells are directly and permanently damaged, the hearing and vestibular recovery cannot be expected. In the barotraumatic PLF, the permanent hearing loss is considered to be caused by homeostatic abnormality from prolonged perilymph leakage not by direct traumatic force to the hair cells.
The management of PLF is still controversial. Conventionally, if a PLF had been clinically suspected, conservative treatment has been considered as a first line management (5, 10). Unless the serviceable hearing was obtained, or if the hearing or vestibular symptoms deteriorated rapidly with a trial of conservative therapy, exploratory tympanotomy and repair of the suspected fistula was considered (3, 7). However, it is very difficult to predict the recovery of hearing impairment at initial or during conservative treatment (11). Progression of hearing loss over time after trauma is common and it may imply that there is continuous leak of perilymph from the fistulous site. Fistula repair to prevent further leakage would prevent further damage of hearing and would increase the chance of functional recovery. Without repair, it would progress to deaf.
In our series, the types of injury are usually barotraumas and less severe head trauma. There were 6 internal trauma and 4 external trauma (2 blunt head trauma from minor car accidents, 2 cheek slap injury). Among the internal trauma, suspected as explosive PLF was 4 (1 heavy lifting, 3 nose blowing) and suspected as implosive PLF was 2 (intense Valsalva maneuver during Yoga). These barotraumas induce perilymph leak by tearing of the RW or OW. Hearing loss will begin from high frequency to progress over time. Dizziness is usually positional vertigo or disequilibrium. The authors think that once the RW or OW is torn, it would be difficult to heal spontaneously, because they are moving and the patients tends to blow their nose to relieve their plugging sensation. If the leakage persists over time, hearing will be worse. Therefore, early surgical repair would be better to prevent the leakage than conservative management.
The optimal indication and timing for surgical treatment remains controversial. Goto et al. (5) suggested that urgent tympanotomy is not required because the surgical closure of a PLF had disappointing results with regard to hearing recovery; in addition, the restoration of disequilibrium was suggested to be the major purpose of the surgical procedure. On the other hand, Seltzer and McCabe (9) reported that improved hearing was possible after many years of symptoms in some patients that underwent PLF repair, and therefore early exploration was suggested to be important. The author's hypothesis is that if a PLF is present, a persistent leak of perilymph could make hearing worse and the inner ear could be irreversibly damaged during the period of conservative management. Therefore, early surgical repair is recommended and waiting several days before exploration in patients with PLF could decrease the probability of hearing recovery. In addition, surgical exploration under local anesthesia has low morbidity and usually takes less than an hour.
In this study, the interval between the traumatic event and surgery was from 2 days to 47 days. However, surgery was performed within two days of the first visit at our center. Because of limited number of cases, conclusions about the optimal timing for improved hearing outcomes after trauma could not be determined. However, there was a trend that showed that earlier surgical repair was associated with greater hearing gains (Fig. 4).
There were a variety of findings at the exploratory tympanotomy among the patients with a suspected PLF. There was no direct evidence of fistula such as definite fistula hole in the RW or OW. However, there were fluid collections in the RW niche (Fig. 3A), bulging of the RW membrane (maybe pseudomembrane) and fibrous web around the RW (Fig. 3C). These findings suggested that the RW was the site of the PLF. Fluid collection and pseudomambrane bulging can be regarded as evident findings of RW fistula. Although fibrous web around the RW can be regarded as non-specific finding, it is unusual finding in normal middle ear and fibrosis can be made by long standing inflammation. In addition, the findings that suggested the OW PLF were a fibrous web around the stapes (Fig. 3B). The types of trauma could be related to the suggested PLF site: the OW or RW (Table 2). For the limited number of cases, there was a tendency that the OW fistula might be more vulnerable to external trauma and RW fistula to internal trauma. It is because the external trauma causes hypermobility of ossicles to subluxate stapes against the OW.
In our series, because of limited number of cases and lacking a control group we could not exactly rule out the effects of conservative management. But despite this, high rate of hearing restoration after early surgical intervention was worthy of notice in suspicious barotraumatic PLF. In conclusion, sudden or progressive sensorineural hearing loss accompanied by dizziness following minor head trauma or barotrauma should raise suspicion for a traumatic PLF. Early surgical exploration is recommended to improve hearing outcomes and control dizziness.