INTRODUCTION
One of the risks in middle ear surgery is high frequency hearing loss. It is believed that manipulations on the middle ear ossicles with the instruments may cause overstimulation of the inner ear and damage of the hear cells. Volter et al. [1] report a significant hearing loss in 0.8% of all middle ear surgery procedures. Tos et al. [2] basing on a large series of 2,300 surgeries due to chronic otitis media reports postoperative high tone hearing loss in 0.7% of patients. Desai et al. [3] report sensorineural hearing loss in 5 from 13 cases (38%) after simple tympanoplasty and 39 from 67 patients (58%) where mastoidectomy was performed.
When myringoplasty is performed in subtotal perforations of the tympanic membrane it is sometimes necessary to separate the tympanic membrane from the handle of the malleus or parts of retraction pockets or cholesteatoma matrix from the incus or malleus [4,5,6]. This would require incision of the handle of the malleus with a sickle knife or a beaver knife and partial elevation of the tympanic membrane from the handle of the malleus. Fisch et al. [4] and Fisch and Linder [5] suggest that separation of the incudostapedial joint (ISJ) prior to further surgical steps of tympanoplasty prevents inadvertent movements of the stapes and thus prevents postoperative high tone hearing loss. He advocates separation of the joint in intact ossicular chain as a surgical step in subtotal perforation myringoplasty. However many other surgeons do not see any advantage in this step [7].
Controversy arises whether temporary separation of the ossicles has any impact on middle ear transfer function and hearing threshold after surgery. Evaluation of this situation in clinical trial would require a group of patients in whom explorative tympanotomy with just separation of the ISJ is performed and another group of patients with explorative tympanotomy only. From obvious reasons such a clinical investigation is not possible. However it may be analyzed in an experimental setup.
The aim of the study is to evaluate the influence of ISJ separation on middle ear function in an experimental model.
MATERIALS AND METHODS
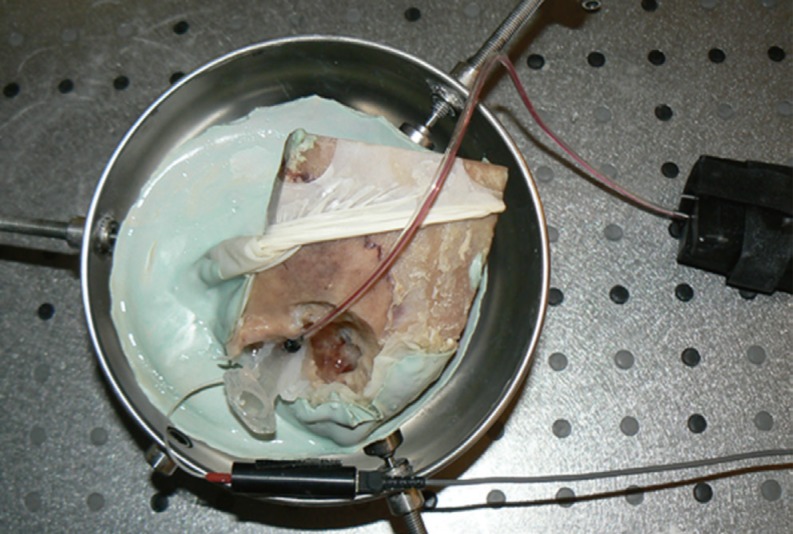
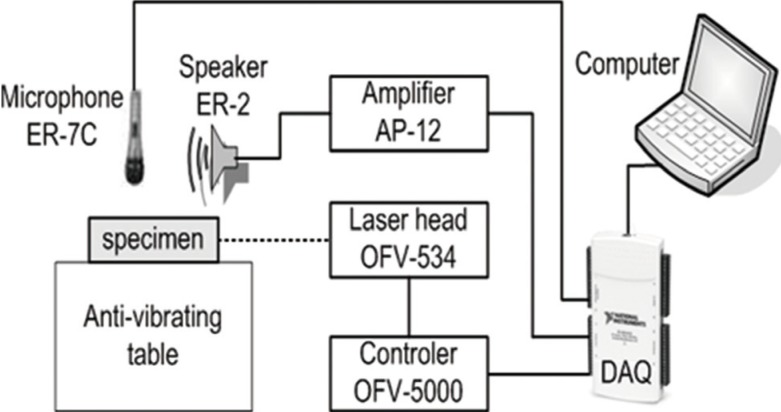
Measurements of stapes vibrations were performed in 5 human temporal bone specimens. The temporal bones were harvested within 48 hours after death and stored in a solution of normal saline with 10 mL of 10% betadine at 5Ōäā between measurements. The soft tissues were removed and a standard antromastoidectomy with posterior tympanotomy performed. The mastoid segment of the facial nerve was removed if necessary to better visualize the stapes arch and the footplate. The ear canal was drilled leaving about 2-3 mm of bone around tympanic annulus. An artificial external ear canal of 25 mm length and 9 mm diameter was then attached to the bone with epoxy resin. The artificial canal had one port for a microphone (ER-7C; Ethymotic Research, Elk Grove Village, IL, USA) and a second port for a sound source (ER2; Ethymotic Reserch) placed about 2 mm from the tympanic membrane. The artificial canal is closed with a glass plate to create a sound seal chamber. One pieces of a retroreflective tape (0.5 mm2 squares), weighing less than 0.05 mg, was placed on the centre of the stapes footplate. The temporal bone specimen was then embedded in dental cement and put in a temporal bone holder (Storz, Tuttlingen, Germany) (Fig. 1). The measurements were performed on antivibration table (Ekspla, Vilnius, Lithuania) inside a sound booth. Vibrations of the ossicles were stimulated by a sound stimuli with a frequency sweeps from 0.2 to 8 kHz at 80-120 dB sound pressure level. The sound source was connected to power amplifier (Interacoustics, Assens, Denmark) to produce an adequate signal output. The stapes footplate velocity and displacement were measured with laser Doppler vibrometer (LDV) system composed of OFV-5000 controller with DD-500 displacement decoder and VD-06 velocity decoder (Polytec, Waldbron, Germany). OFV-534 sensor head was connected to a joystick operated micromanipulator, which was mounted on the operating microscope (Zeiss, Jena, Germany). The helium-neon laser beam was directed with the micromanipulator onto stapes footplate through posterior tympanotomy. The experimental setup is showed in Fig. 2. The measurements have been recorded using processing board NI6210 (National Instruments, Austin, TX, USA) and DasyLab software and then the experimental data analysed with the MatLab package. Only measurements with signal to noise ratio better than 10 were accepted. Velocity of the stapes footplate was normalized to sound pressure level measured in the ear canal.
The measurements of stapes vibration were performed in an intact ossicular chain and again after ISJ separation with Rosen knife or 90 degree angled 1.5 mm microhook. After sectioning of the joint the lenticular process was resting on the stapes head. Both ossicles were attached to each other only by fluid adhesion. Care was taken not to luxate the incus nor stapes during ISJ separation. The study was approved by Institutional Ethical Committee.
RESULTS
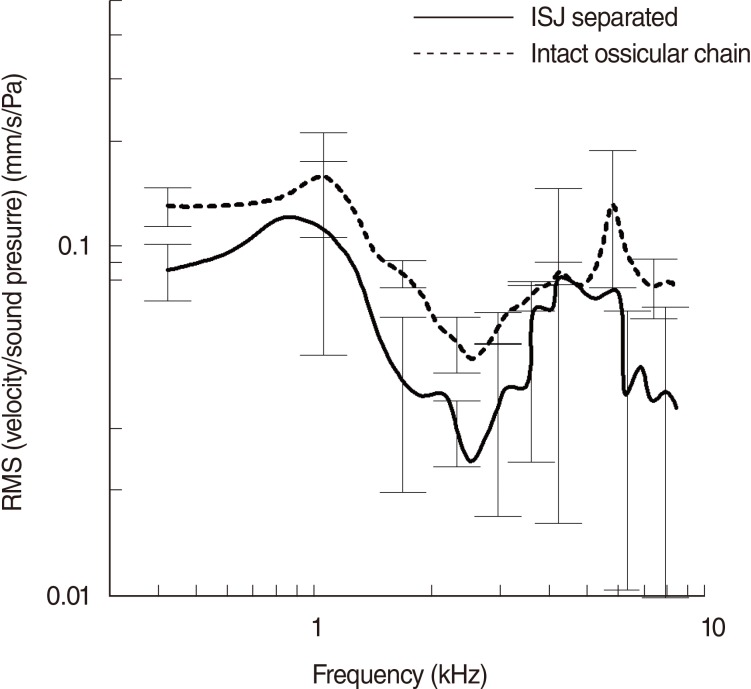
In all cases there was a decrease in stapes velocity after ISJ separation. Mean stapes velocity was reduced for 1 dB in 800 Hz to 9 dB in frequencies above 1,000 Hz. The decrease of velocity was greater in higher frequencies. The results of measurements are depicted in Fig. 3.
DISCUSSION
Proper understanding of mechanism of ISJ function requires a good knowledge of its architecture. Chien et al. [8] analysed the anatomy of ISJ in histologic section of human temporal bones. They showed that the lenticular process has narrow bony pedicle and flat osteocartilaginous plate. The ISJ consists of a narrow space lined by synovium between cartilaginous surfaces of the stapes head and lenticular plate. The outer surface of the joint is covered by a fibrous capsule. In about 80% of specimens analysed by Chien et al. [8], a fibrocartilaginous disc was visible between synovial surfaces of the ISJ. Lenticular process demonstrates areolar tissue-filled spaces. Those scalloped areas of lenticular process contain fibers of the joint capsule. Similar findings were observed by Karmody et al. [9]. They studied anatomy of the ISJ in histologic sections in 86 human temporal bones. Joint capsule is attached to the full length of the lenticular process and extends medially to the rim of the stapes head.
Separation of the ISJ is usually performed with a sharp plate knife or 90 degree hook. Delicate movements of the incus with an instrument usually creates a line where the joint capsule bends. This helps to locate the place for incision of the joint.
During ISJ separation there is a risk of damaging the lenticular process especially in cases where its pedicle is very thin. In such situation a reconstruction is necessary resulting in possible conductive hearing loss.
The ISJ plays an important role in atmospheric pressure changes in the middle ear. In negative middle ear pressure the malleus is moving medially but the incus inferiorly causing stapes rotation along its long axis [10].
Vlaming and Feenstra [11] analysed in temporal bone specimens stiffness of the middle ear with the use of LDV. They concluded that the dumping effect of the normal ear is located mainly at the stapes footplate to cochlea level and that the ossicles do not contribute significantly to the total stiffness of the middle ear. It seems that the complete capsule of the ISJ may be more important in adaptation to static pressure changes in the middle ear than in sound vibration.
The integrity of the ISJ is necessary for a proper sound conduction. In cases of head trauma with incus dislocation significant hearing loss may develop. It is mainly because the dislocated incus after trauma is not in physiological position. The surfaces of the ISJ are usually separated and need to be approximated and supported [12,13,14]. In temporary ISJ separation during middle ear surgery the position of the ossicles is intact thus it does not require any reconstruction. In cases where lenticular process has been damaged or inxus luxated appropriate reconstruction in necessary. Several possible techniques are possible including bone cement bridging, incus interposition or joint prosthesis use [15].
Separation of the ISJ has not reduced significantly middle ear transfer function in our experimental model. The ISJ in patients after temporary separation is subjected to healing processes. Therefore we assume that the stapes vibration after healing in humans would be even better than in our experimental model. On the other hand the healing process can potentially lead to ankylosis which would result in conductive hearing loss.
There is still an open question whether separation of the ISJ can prevent high frequency hearing loss. Surely, when ISJ is separated the incus is more mobile so any manipulations on it may temporary create a gap between ossicles thus preventing high stimulation of the cochlea. It is also possible to elevate slightly malleus or incus for the time of manipulations and disconnect surfaces of the joint. This however may also carry the risk of luxation of the ossicles. Other factors like suction or drilling may also contribute in postoperative hearing loss making any clinical analysis very difficult [15,16,17].
The decision whether to divide or not the ISJ should be made taking into account the amount of manipulation on the ossicles planned and the risk of damage of the joint.
In conclusion, separation of the ISJ does not reduce significantly the middle ear function.