INTRODUCTION
Sleep-disordered breathing (SDB), such as snoring or obstructive sleep apnea (OSA) is characterized by repeated narrowing or collapse of the upper airway during sleep. Surgical modifications of the upper airway have an important role in the treatment of patients with SDB because anatomical factors may contribute to the development or aggravation of SDB [1].
Among the various surgical procedures for SDB, laser-assisted uvulopalatoplasty (LAUP) was broadly performed for the treatment of snoring or OSA in the 1990s [2,3]. However, LAUP is not presently recommended for the treatment of SDB including OSA due to insufficient evidence on its efficacy [4].
It has been reported that palatal implants may help to improve persistent or recurrent SDB including snoring and mild to moderate OSA after uvulopalatopharyngoplasty (UPPP) or LAUP; however, the success rate (defined as a greater than 50% reduction in preoperative apnea-hypopnea index [AHI] and a postoperative AHI of less than 20) of palatal implants following failed palatal surgery is relatively very low and the cure rate (defined as a postoperative AHI of less than 5) is unknown [5,6].
Here we report a case of curative therapy with the Pillar palatal implant procedure (Medtronic, Minneapolis, MN, USA) for persistent snoring and mild OSA after LAUP.
CASE REPORT
A 56-year-old man visited our hospital with a 15-year history of persistent snoring and witnessed apnea after LAUP. His subjective snoring level was six on a seven-point Liker scale ranging from 0 (none of the time) to 6 (all of the time). He had no relevant medical history, including hypertension, diabetes mellitus, or stroke. Body mass index (BMI) was 24.8 kg/m2 (height was 162 cm and weight was 65 kg).
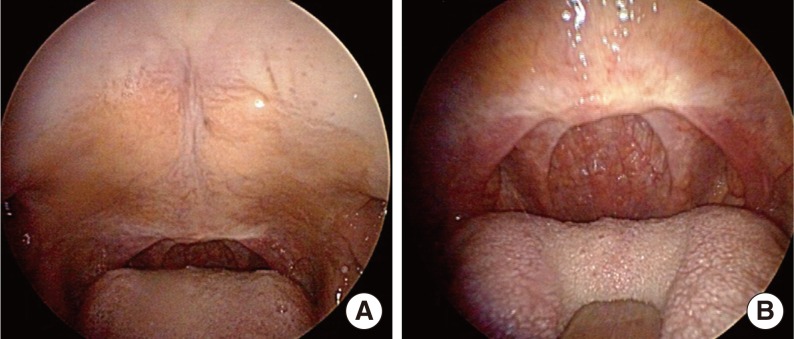
On direct examination of the oral cavity and oropharynx, the uvula was not observed because of the previous surgical procedure (Fig. 1). Palatine tonsils were small (hidden within the pillars), and the Friedman tongue position was presumed as grade 2 [7]. The soft palate length was longer than 2.5 cm, and nasopharyngeal stenosis was not found. Retropalatal obstruction was suspected based on physical examination and the Muller maneuver.
He was diagnosed with mild OSA based on diagnostic standard (overnight, attended, laboratory-based) polysomnographic results (AHI=7.6 events/hour [supine AHI=13.7 events/hour and non-supine AHI=0.6 events/hour], apnea index [AI]=0.8 events/hour, minimum SaO2=91%, arousal index=23.8 events/hour, and snoring=51.3%).
Continuous positive airway pressure (CPAP) or oral appliance (OA) was recommended as a primary therapy. However, he was unwilling to accept CPAP or OA as a permanent solution and chose to undergo an alternative minimally invasive surgical treatment.
A palatal stiffening procedure using the Pillar palatal implant procedure was performed under local anesthesia according to the following simple steps: (1) determine three palatal implant insertion sites and inject with local anesthetic agent on surgical fields; (2) insert the needle of the delivery system through the sub-mucosal tissue layer into the muscle and place the implants in the muscular layer of the palate (three implants were located at about 2 mm intervals); (3) withdraw the needle and inspect the palatal mucosal surface (oral and nasopharyngeal) to ensure the implants were properly placed. There were no specific perioperative complications except mild discomfort at the operative site.
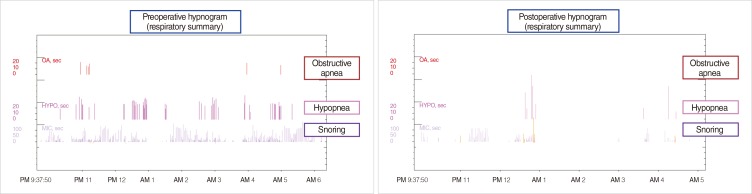
Two months after the Pillar procedure, subjective snoring level decreased from 6 to 2 and follow-up standard polysomnographic results (AHI=1.3 events/hour [supine AHI=2.3 events/hour and non-supine AHI=0.3 events/hour], AI=0.0 events/hour, minimum SaO2=90%, arousal index=18.9 events/hour, and snoring=16.8%) were clearly improved compared to those of the preoperative sleep test (Fig. 2). BMI was 23.6 kg/m2 (body weight was 62 kg) at two months following the procedure. Mild discomfort at the operative site resolved without morbidity, and postoperative complications such as extrusion or infection were not observed.
DISCUSSION
LAUP, introduced by Kamami [2] in 1990, has been a popular procedure for the treatment of snoring and/or mild OSA. However, there continues to be a controversy about the efficacy of LAUP in patients with SDB including OSA [3,8]. Recent practice parameters of the American Academy of Sleep Medicine state that LAUP is not routinely recommended for the management of OSA because there is no significant postoperative improvement and there is the possibility of complications or side effects [4].
After previous palatal surgery, persistent or recurrent snoring and/or OSA may be caused by retroglossal obstruction and/or retropalatal obstruction due to inadequate widening. According to several studies, persistent retropalatal obstruction seems to play a prominent role in some patients with residual SDB after UPPP [9,10].
To our knowledge, two studies have focused specifically on alternative surgeries in patients who refuse primary medical treatment including CPAP and OA after failed palatal surgery [5,6]. Friedman et al. [5] prospectively evaluated the effects of palatal stiffening using palatal implants on subjective and objective improvements in 23 selected patients with persistent or recurrent snoring and mild to moderate OSA after UPPP or LAUP. They found that there was a significant improvement in subjective snoring, AHI, and minimum oxygen saturation. However, in their study, the success rate was relatively low (5/23, 21.7%) and the cure rate was not mentioned. In addition, there was no description about the surgical result after palatal implants for failed LAUP group alone. O'Connor-Reina et al. [6] conducted a prospective, nonrandomized study of 16 non-severe SDB patients treated with palatal implants after failed UPPP and found that subjective snoring and AHI were significantly improved. However, the success or cure rate of the palatal implant procedure was very low in the comparison between preoperative and postoperative AHI.
Palatal implants as well as most other palatal surgeries may be effective in some patients with mild OSA [4]. However, to increase the success rate, the identification of appropriate surgical candidates is very important. General guidelines for identifying favorable surgical candidates for palatal implants after failed UPPP or LAUP include [5,6]: (1) age≥18 years; (2) BMI<25 kg/m2; (3) simple snorer or mild OSA (AHI<15 events/hour); (4) retropalatal obstruction suspected based on physical examination (tonsil size, palate-tongue position, etc.), Muller maneuver, or sleep endoscopy (no evidence of retroglossal obstruction); (5) residual soft palatal length≥2 cm; (6) no nasopharyngeal stenosis; (7) unwillingness to accept CPAP or OA as a long-term, permanent solution; and (8) willingness to accept possible perioperative or postoperative risks.
Two months after the procedure, body weight decreased by 3 kg (4.6%). According to the previous study, a 5% weight loss predicted a 14% reduction in the AHI [11]. In this case, AHI reduced by 82.9% (from 7.6 to 1.3 events/hour) after palatal implants. Body weight reduction may slightly influence postoperative AHI. However, we think that the effect of weight loss on AHI is minimal in this case.
In conclusion, this case indicates that palatal implants may be offered as an alternative minimally invasive palatal surgery in selective patients with persistent or recurrent snoring and/or mild OSA after LAUP.