|
 |
- Search
AbstractObjectivesTo show that mechanical compression of sigmoid sinus is effective for treatment of pulsatile tinnitus caused by sigmoid sinus enlargement, and to evaluate the relationship between the compression degree of sigmoid sinus and the tinnitus symptom relief using magnetic resonance angiography.
MethodsMedical records of twenty-four patients who were diagnosed with venous tinnitus caused by sigmoid sinus enlargement and underwent mechanical compression of sigmoid sinus were reviewed between April 2009 and May 2013. All these patients received computed tomography and magnetic resonance venography study before undergoing surgery and were followed for at least 4 months.
ResultsTwenty-three patients felt relief from tinnitus three months after the surgery, and the cross-sectional area of the sigmoid sinus on the tinnitus side was compressed approximately by half (46%-69%) after the surgery. There were 4 patients whose tinnitus suddenly disappeared while lying on the operating table before operation, which may be a result of the patient's emotional tension or postural changes from standing. One of the four patients felt no relief from tinnitus after the surgery, with the cross-sectional area of the sigmoid sinus only compressed by 30%. And two patients of them had a recurrence of tinnitus about 6 months after the surgery. Seven patients had sigmoid sinus diverticula, and tinnitus would not disappear merely by eliminating the diverticulum until by compressing the sigmoid sinus to certain degree. There were 3 minor complications, including aural fullness, head fullness and hyperacusis. The preoperative low frequency conductive and sensorineural hearing loss of 7 subjects subsided.
ConclusionMechanical compression of sigmoid sinus is an effective treatment for pulsatile tinnitus caused by sigmoid sinus enlargement, even if it might be accompanied by sigmoid sinus diverticulum. A compression degree of sigmoid sinus about 54% is adequate for the relief of tinnitus symptom. Cases in which patients' tinnitus suddenly disappeared before the surgery might be excluded to improve the efficacy of surgery.
Pulsatile tinnitus (PT) generates by vascular or other structures within the cranial cavity, head and neck region, and thoracic cavity, and it is transmitted to the cochlea by bony or vascular structures. PT could be caused by either increased blood flow or stenosis of a vascular lumen and can be classified as arterial or venous according to the vessel of origin [1]. Venous PT is more common [2] and may result from primary venous anomalies, increased intracranial pressure and transmission of arterial pulsations to the dural venous sinuses [3]. Augmented or turbulent flow within the transverse-sigmoid-jugular venous system is one of the most common causes of venous PT [4].
Persistent venous PT would have serious impact on the quality of the patients' daily life. Clinicians [4,5,6] had tried to bring relief from PT through ligating jugular vein in the neck, but it would trigger florid pseudotumor cerebri that might be accompanied by severe headaches, progressive visual loss, and other disturbing neurologic symptoms [4], especially when it comes to stenosis or atresia of the contralateral system. With the technology advancement, magnetic resonance venography (MRV) has been applied to study the intracranial venous morphology and drainage situation, and venous malformations referred to as aneurysms or diverticula of transverse-sigmoid sinus or arteriovenous fistula (AVF) have been diagnosed and treated in the existing literatures [7,8,9]. In our study, twenty-four subjects diagnosed with venous PT underwent the MRV study, and all subjects were found having unilateral dominant sigmoid sinus and internal jugular vein but without those venous malformations mentioned above, such as aneurysms and AVF.
In this study, series of PT patients treated with mechanical compression of sigmoid sinus in China is reported, and indications and outcomes of the procedure are reviewed. Pearls and pitfalls are noted to facilitate appropriate and effective application of this technique to patients with PT caused by sigmoid sinus enlargement.
A retrospective medical chart review between April 2009 and May 2013 was conducted at the Eye Ear Nose and Throat Hospital of Fudan University (Shanghai). Information related to patient demographics, indications, intraoperative findings, changes of the cross-sectional area of sigmoid sinus, complications and outcomes was collected. The Ethics Review Board of the Eye Ear Nose and Throat Hospital of Fudan University approved the study and written informed consent was obtained from all participants.
All patients in this series had undergone physical examination, including otoscopic examination and pure-tone audiometry test. A high resolution temporal bone computed tomography (HRTBCT) scan was used to identify bony/developmental of the middle ear and sigmoid sinus; the magnetic resonance (MR) angiography was performed on MAGNETOM Verio 3.0-T (Siemens AG, Muenchen, Germany) scanners, using a contiguous 2-dimensional time-of-flight MR angiographic technique and an inferior saturation band, to eliminate signal from arterial structures. Sections with a thickness of 2.5 mm were acquired in the axial plane when parameters were set to be: 21.0/5.0 (TR/TE), 60┬░ flip angle, and 272*320 matrix. We used the software NUMARIS/4 (SYNGO MR B17, Siemens AG) to measure the cross-sectional area of the sigmoid sinus, and the average of 3 maximum values was obtained for comparison between the healthy side and the tinnitus side. On the third day after the operation, we measured the cross-sectional area of the center plane of the compressed sites and made a 3-dimensional reconstruction of the sigmoid sinus. MRV can help to understand the blood flow condition of the sigmoid sinus. If there was a perceived alteration in the blood stream, the blood stream signal on MRV would not be enhanced, then we recorded this condition as "yes," otherwise it was recorded to be "no."
We used the visual analogue scale to assess the severity of tinnitus, with 1-3 points indicating mild tinnitus, 4-7 points indicating moderate tinnitus, and 8-10 points indicating severe tinnitus.
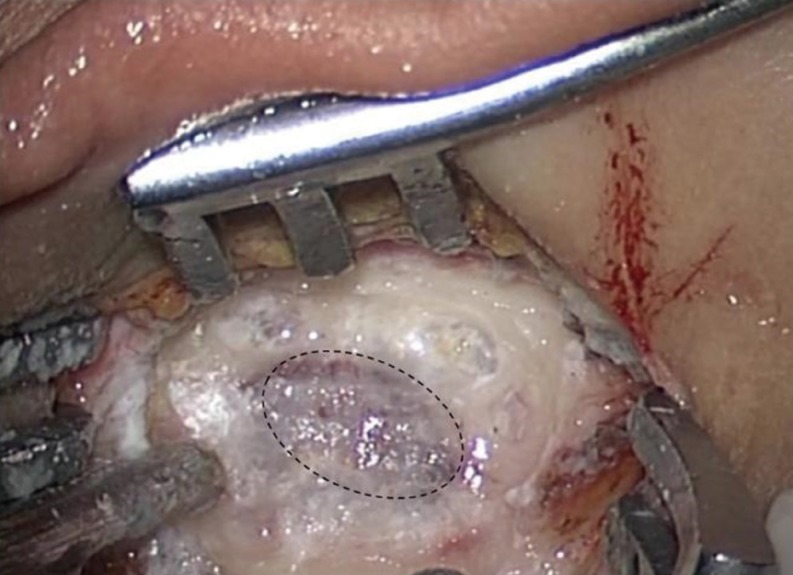
The procedure with mechanical compression of sigmoid sinus was performed under regional anesthesia. Subjects were lying on the operating table in the otological surgery position. The lateral bone of the sigmoid sinus was cut, without invading the mastoid air cells system as far as possible. The surgery was performed to expose the most prominent site of the sigmoid sinus directed by the imaging studies. About 1.5├Ś1.0-cm2 area of the prominent sigmoid sinus was exposed (Fig. 1). Then the prominent sigmoid sinus was compressed slowly and subjects were asked whether tinnitus disappeared or not. When the subjects said that tinnitus disappeared, right compressing depth was obtained (Fig. 2). After that, auricular cartilage, temporalis muscle and fascia were harvested and were inserted into the bony bridge (Fig. 3), which was fixed by octyl-cyanoacrylate/N-butyl-cyanoacrylate (Stryker Corp., Kalamazoo, MI, USA).
Twenty-four subjects (23 females, 1 male) underwent mechanical compression of sigmoid sinus. The average age of the female patients was 40 (ranging from 29 to 61), and the male patient was 23 years old. The duration of PT for all patients varied from 6 months to 11 years, and otoscopic examination revealed no middle ear abnormalities in them. Pure-tone audiometry test of 17 patients was normal, but 3 patients showed bilateral mild conductive hearing loss in the low frequencies, and four patients showed mild unilateral sensorineural hearing loss in the low frequencies. There were no history of head or neck trauma, cardiovascular disease or ear surgery, papilledema, hypertension, diabetes mellitus, and thyroid disease for all patients. All subjects had been diagnosed with venous PT at first. HRTBCT results showed all patients had sigmoid sinus enlargement, and in the meanwhile 7 patients had sigmoid sinus diverticula. Among the 24 patients, MRV showed 19 of them had a right-sided dominant sigmoid sinus and internal jugular vein, and 5 had a left-sided dominant sigmoid sinus and internal jugular vein.
During the operation, the surgeon found 7 patients had small sigmoid sinus diverticula. The diverticula were skeletonized and compressed to a normal-appearing sinus to eliminate the audible turbulence, but tinnitus did not disappear merely by eliminating the diverticulum until the dominant sigmoid sinus was compressed to certain degree. Four patients (Table 1) said tinnitus disappeared when they lay on the operating table before compressing sigmoid sinus; for no other PT causes were identified, so the surgery was still performed, though the surgeon could not determine the appropriate compression degree.
The patients who were diagnosed with PT caused by sigmoid sinus enlargement underwent mechanical compression of sigmoid sinus, and the cross-sectional area of the sigmoid sinus in the tinnitus side was about two times (ranging from 1.89 to 6.9 times) of that of the healthy side. Seventeen patients said their tinnitus disappeared and 6 patients reported that the tinnitus was reduced. The cross-sectional area of the sigmoid sinus of the 23 patients was compressed by 46% to 69% (Fig. 4A-C). Only one patient's treatment turned out to be ineffective, whose cross-sectional area of the sigmoid sinus was compressed by 30%. Fourteen patients' blood stream signal was recorded as "yes" before the surgery, while only two patients' blood stream signal still remained "yes" after the operation (Table 1).
We think that it is necessary to mention a female subject (Table 1), whose tinnitus disappeared after the surgery but she had persistent headache and eye pain approximately two weeks after the surgery. MRV of the brain demonstrated that the sigmoid sinus was almost completely obstructed due to expansion of the gelatin sponge. During the process of surgery, gelatin sponge was used as a temporary filling material for lacking filler material. However, the volume of gelatin sponge expanded and hardened when it encountered and reacted with blood and brain glue. The symptoms mentioned above disappeared after the expanded and hardened gelatin sponge was removed through reoperation. Then the sigmoid sinus was compressed by 49%, and tinnitus was better reduced than the first surgery.
Three patients had aural fullness and were found having hemotympanum by otoscopic examination one day after the surgery. One patient had head fullness but no papilledema was found by ophthalmoscope examination two days after the surgery. The ear fullness and head fullness of patients disappeared about two weeks after the operation. Two patients had mild hyperacusis one month after the operation. Others had no relevant serious complications.
One month after the operation, all patients received audiometry. The efficacy of the surgery was reinforced by the improvement of the preoperative low frequency conductive and sensorineural hearing loss. It turned out that the low frequency hearing loss was caused by the masking effect of the PT.
Follow-up time of all subjects ranged from 6 months to 56 months. Two patients had tinnitus recurrence about 6 months after the surgery and it was the two patients that had reported their tinnitus suddenly disappeared before the surgery.
PT needs to be evaluated thoroughly. Failure or delay in the diagnosis, or misdiagnosis may have disastrous consequences. MR angiography and computed tomography (CT) are useful for diagnosing anatomical abnormalities that may contribute to PT [10]. Reasonable application of imaging examination would rule out the pathological causes of PT: jugular glomus, paraganglioma, AVF, acquired stenosis or aberrant course of the internal carotid artery, carotid-cavernous fistulae, benign intracranial hypertension (BIH), dehiscent jugular bulb, diverticulum, aneurysms, vascular loop in the internal auditory canal and head and neck arterio-venous malformations [2,3,9,10,11]. In our study, all subjects underwent MRV/CT study and had been diagnosed with sigmoid sinus enlargement, but no other abnormalities mentioned above were found in them. The sound that all subjects heard was coincident with their heartbeat. The sound intensity decreased during a light digital compression of the ipsilateral neck vein or with the head turning to the tinnitus side, and the sound intensity increased with the head turning to the contralateral side. So, all subjects were diagnosed with venous PT caused by sigmoid sinus enlargement.
Sismanis has reported BIH is the most common cause (56/145) of PT and has a large female preponderance [12]. For young obese women with blurred vision, headaches and papilledema, a diagnosis of BIH may be established by lumbar puncture after magnetic resonance imaging (MRI) [3,10]. And empty sella was the main MRI or CT examination results for BIH [13]. Meanwhile in our study, twenty-three of the twenty-four patients were females. Though all patients complained of heart-beat sound, no blurred vision, headaches and papilledema were found, and associating with the imaging study results, we believed that no one was diagnosed with BIH.
Madani and Connor [14] reported that the prevalence of dural arteriovenous fistula (DAVF) in patients with PT was variably high up to 20%. DAVF involving the sigmoid sinus and transverse sinus was more common [9]. MRI/magnetic resonance angiography was much more sensitive to the detection of transverse or sigmoid sinus DAVF [10]. The natural history of DAVFs that drain directly into a dural venous sinus with normal antegrade flow is now known to be benign and the chance of stability or spontaneous symptom resolution is high [15]. In our study, four patients said tinnitus spontaneously disappeared when they lay on the operation table before mechanical compression of the sigmoid sinus was performed. Based on the four patient's imaging study results and clinical examination, DAVFs could be ruled out. We assumed that the disappearing of tinnitus may be relevant with the patients' emotional tension or their postural changes from standing, for these two factors maybe lead to changes in blood flow around the ear, resulting in tinnitus changes. For these patients, especially two patients who had recurrence of tinnitus after the surgery, their tinnitus may be affected by a variety of factors. Therefore, if the two patients' tinnitus is treated only by mechanical compression of sigmoid sinus, the surgical effect may be limited.
In recent years, several cases were reported, in which PT was said to be caused by diverticulum or aneurysm of the sigmoid sinus. Mattox and Hudgins [2] had reported that the most common abnormality of the venous system identified was sigmoid sinus diverticula, which turned out to be the cause of PT in 11 of 54 patients (20%). The endoluminal embolization approach and transmastoid extraluminal approach make PT decrease or disappear [7,8]. The literatures [8,16] indicate that the sigmoid sinus diverticulum could result in PT and removing the diverticulum could make PT decrease under general anesthesia. However, it was hard to determine the relationship between the elimination of diverticulum and the decrease of PT when general anesthesia was conducted. Mechanical compression of sigmoid sinus in this paper was performed under local anesthesia. The surgeon found that 7 patients had small sigmoid sinus diverticulum, and tinnitus did not disappear merely by eliminating the diverticulum, and it disappeared until the prominent sigmoid sinus was compressed to certain degree. This indicates that the typical dominance of the venous drainage system does play an important role in the pathogenesis of PT, but sigmoid sinus diverticulum can only show the deformation degree of the sigmoid sinus.
The anatomic preponderance of the right sigmoid sinus is common [17]. Krishnan et al. [13] had declared that only ipsilateral dominance of the venous system could be identified as a potential cause of PT. Cho et al. [18] agreed that unilateral dominant size of the venous system may cause PT, and also found that the largest area/smallest area (L/S) ratio>4.75 may be a criterion indicating abrupt caliber change and causing PT. In our study, there was a strong prevalence favoring the right ear in this series, with 19 of 24 ears treated on the right. And there were 5 cases of PT on the left all had ipsilateral dominant venous drainage. In addition, we found that the average cross-sectional area of the sigmoid sinus on the tinnitus side is about 2.64 times wider than that of the healthy side (ranging from 1.89 to 6.9).
There was little literature reporting PT treatment through compression of sigmoid sinus. Wee et al. [19] had reported a successful case that PT caused by a prominent sigmoid sinus was markedly improved by compressing sigmoid sinus, compressing approximately half of the cross-sectional diameter of the sigmoid sinus. In our study, twenty-three of the twenty-four patients were relieved of PT. And the cross-sectional area of the sigmoid sinus on the tinnitus side was compressed about by 54% (ranging from 46% to 69%). Only one patient's tinnitus was not improved, whose cross-sectional area of the sigmoid sinus on the tinnitus side was compressed about by 30%, which was too little to decrease the tinnitus caused by prominent sigmoid sinus.
In this study, there were mainly three kinds of postoperative complications: aural fullness, head fullness, and hyperacusis. Postoperative aural fullness may result from the hemotympanum after the transmastoid surgery. Due to lacking evidence of intracranial hypertension, head fullness may result from the temporary disturbance of venous return. When blood reconstruction was completed, head fullness would be relieved. The reason for hyperacusis was still unclear. Wee et al. [19] published a pulsating headache after the sigmoid sinus was almost completely obstructed. Only by decompressing the sigmoid sinus can the venous flow be recovered, and the patient's headache would subside. In this study, gelatin sponge used as filling materials obstructed the sigmoid sinus, so we must strictly choose filling material and reserve partial blood flow rather than completely obstructing the sigmoid sinus. It is necessary to monitor patients' postoperation conditions, considering the reported morbidity associated with surgical alteration of intracranial blood flow.
In conclusion, mechanical compression of sigmoid sinus is an effective treatment for PT caused by sigmoid sinus enlargement, even if accompanied by the sigmoid sinus diverticulum. The typical dominance of the venous drainage system is the pathogenesis of PT. Compressing the cross-sectional area of the sigmoid sinus approximately by 54% can keep the venous blood flow, and can also achieve better treatment effect. The patients whose tinnitus suddenly disappeared before the surgery might be excluded to improve the efficacy of surgery.
CONFLICT OF INTERESTCONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported. References2. Mattox DE, Hudgins P. Algorithm for evaluation of pulsatile tinnitus. Acta Otolaryngol. 2008 4;128(4):427-431. PMID: 18368578.
3. Sismanis A. Otologic manifestations of benign intracranial hypertension syndrome: diagnosis and management. Laryngoscope. 1987 8;97(8 Pt 2 Suppl 42):1-17. PMID: 3302575.
4. Jackler RK, Brackmann DE, Sismanis A. A warning on venous ligation for pulsatile tinnitus. Otol Neurotol. 2001 5;22(3):427-428. PMID: 11347652.
5. Aikoye AA, Tang TY, Meyer FJ. Local anaesthetic surgical treatment of severe objective pulsatile tinnitus: a useful technique. Ann R Coll Surg Engl. 2012 5;94(4):e139-e140. PMID: 22613279.
6. Golueke PJ, Panetta T, Sclafani S, Varughese G. Tinnitus originating from an abnormal jugular bulb: treatment by jugular vein ligation. J Vasc Surg. 1987 9;6(3):248-251. PMID: 3625880.
7. Santos-Franco JA, Lee A, Nava-Salgado G, Zenteno M, Vega-Montesinos S, Pane-Pianese C. Hybrid carotid stent for the management of a venous aneurysm of the sigmoid sinus treated by sole stenting. Vasc Endovascular Surg. 2012 5;46(4):342-346. PMID: 22534612.
8. Otto KJ, Hudgins PA, Abdelkafy W, Mattox DE. Sigmoid sinus diverticulum: a new surgical approach to the correction of pulsatile tinnitus. Otol Neurotol. 2007 1;28(1):48-53. PMID: 17195746.
9. Park IH, Kang HJ, Suh SI, Chae SW. Dural arteriovenous fistula presenting as subjective pulsatile tinnitus. Arch Otolaryngol Head Neck Surg. 2006 10;132(10):1148-1150. PMID: 17043268.
10. Shin EJ, Lalwani AK, Dowd CF. Role of angiography in the evaluation of patients with pulsatile tinnitus. Laryngoscope. 2000 11;110(11):1916-1920. PMID: 11081610.
11. De Ridder D, De Ridder L, Nowe V, Thierens H, Van de Heyning P, Moller A. Pulsatile tinnitus and the intrameatal vascular loop: why do we not hear our carotids? Neurosurgery. 2005 12;57(6):1213-1217. PMID: 16331169.
12. Sismanis A. Pulsatile tinnitus: a 15-year experience. Am J Otol. 1998 7;19(4):472-477. PMID: 9661757.
13. Krishnan A, Mattox DE, Fountain AJ, Hudgins PA. CT arteriography and venography in pulsatile tinnitus: preliminary results. AJNR Am J Neuroradiol. 2006 9;27(8):1635-1638. PMID: 16971601.
14. Madani G, Connor SE. Imaging in pulsatile tinnitus. Clin Radiol. 2009 3;64(3):319-328. PMID: 19185662.
15. Davies MA, Saleh J, Ter Brugge K, Willinsky R, Wallace MC. The natural history and management of intracranial dural arteriovenous fistulae. Part 1: benign lesions. Interv Neuroradiol. 1997 12;3(4):295-302. PMID: 20678360.
16. Eisenman DJ. Sinus wall reconstruction for sigmoid sinus diverticulum and dehiscence: a standardized surgical procedure for a range of radiographic findings. Otol Neurotol. 2011 9;32(7):1116-1119. PMID: 21799456.
17. Duvillard C, Ballester M, Redon E, Romanet P. Pulsatile tinnitus cured by mastoidectomy. Ann Otol Rhinol Laryngol. 2004 9;113(9):730-733. PMID: 15453531.
18. Cho IK, Jung JY, Yoo DS, Suh MW. 3-Dimensional reconstruction of the venous system in patients suffering from pulsatile tinnitus. Acta Otolaryngol. 2012 3;132(3):285-289. PMID: 22200123.
19. Wee JH, Song JJ, Koo JW, Kim CS. Increased intracranial pressure after surgical treatment of pulsatile tinnitus from a prominent sigmoid sinus. Otol Neurotol. 2012 8;33(6):e41-e42. PMID: 22334154.
Fig.┬Ā2The prominent sigmoid sinus was being compressed and meanwhile the subject was asked whether tinnitus disappeared or not.
Fig.┬Ā3After application of auricular cartilage, temporalis muscle fascia and octyl-cyanoacrylate/N-butyl-cyanoacrylate.
Fig.┬Ā4Preoperative temporal bone computed tomography (A, arrow) and magnetic resonance venography (B, arrow) showing an enlargement of right sigmoid sinus. Postoperative magnetic resonance venography demonstrating 56% surgical compression of sigmoid sinus (C, arrow).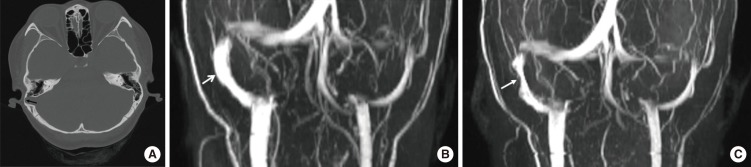
Table┬Ā1.Tinnitus and sigmoid sinus changes of the patients
Pre, preoperative; post, postoperative; VAS, visual analogue scale; T, tinnitus side; H, health side; S, uneven signals; TP, postoperative health side; T/H, sigmoid sinus enlargement; T-TP/T, sigmoid sinus narrowed degree, CT, computed tomography; SSD, sigmoid sinus diverticulum. |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||