INTRODUCTION
Leukemia frequently gives rise to otologic signs and symptoms in several ways, the most common being the infiltration of leukemic cells, which results in small hemorrhages and infections of the ear (1, 2). Very rarely, however, otologic symptoms result from myeloid sarcoma, which is a discrete mass composed of malignant myeloid cells.
To date, there have been only a few case reports of myeloid sarcoma involving the temporal bone. Five such patients were recently seen and treated at our institution. In this report, we examine the clinical features of myeloid sarcoma involving the temporal bone by comparing its clinical features with those of metastatic lesions of the temporal bone and the lesions originate from non-systemic malignancy. All of the clinical features of these five cases are summarized in Table 1.
CASE REPORTS
Case 1
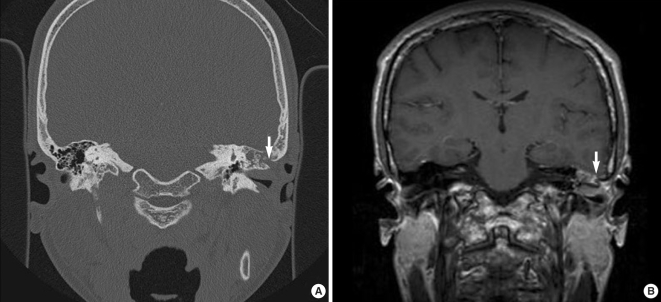
A 21-yr-old male presented with left-side ear fullness of 1 month's duration. He had been previously treated for otitis externa at a local clinic. Six years earlier, he was diagnosed with acute myeloid leukemia (M1) and underwent bone marrow transplantation after achieving complete remission. On physical exam, the posterosuperior part of the external auditory canal (EAC) showed marked bulging and the tympanic membrane was not visible. Pure-tone audiometry showed a left-side conductive hearing loss of 35 dB. A computed tomography (CT) scan of the temporal bone showed a soft-tissue density filling the mastoid antrum and middle ear. The soft tissue had eroded the mastoid cortex and seemed to extend to the wall of the EAC. Magnetic resonance imaging (MRI) of the temporal bone showed similar results (Fig. 1). A pathologic study of the EAC mass confirmed the diagnosis as myeloid sarcoma. Bone marrow biopsy showed relapsing leukemia. Unfortunately, the patient died of septic shock 1 month into a course of chemotherapy.
Case 2
A 47-yr-old male with left facial palsy and retroauricular swelling was referred to our institution after being seen at another hospital for facial palsy, which had begun 3 months earlier. However, his symptoms had not improved and retroauricular swelling had developed on the same side 1 month before he came to our attention.
One year earlier, he was diagnosed with acute myeloid leukemia (AML), type M2, obtaining complete remission after chemotherapy. He denied a history of trauma, upper respiratory tract infection, or previous facial palsy. On physical exam, the left tympanic membrane was intact, but the posterior wall of the EAC bulged and a retroauricular swelling of about 10 cm was seen. MRI of the temporal bone showed a poorly demarcated, homogenously enhancing soft-tissue density filling the subcutaneous layer over the mastoid cortex, and forming a large mass around the mastoid tip (Fig. 2). The mastoid antrum was partially filled with the soft-tissue density. However, a connection between the mastoid and the subcutaneous mass could not be determined, nor was there evidence of facial nerve invasion by the mass. Biopsy to evaluate the mass confirmed a diagnosis of myeloid sarcoma. Bone marrow biopsy studies revealed no evidence of leukemia relapse. During radiotherapy, the facial palsy improved temporarily but then worsened and a relapse of leukemia was diagnosed on a repeat bone marrow biopsy after 3 months. During treatment for relapsing leukemia, the patient died from septic shock.
Case 3
A 12-yr-old boy visited our clinic due to a left-side retroauricular swelling of 2 months duration. He had been diagnosed with AML (M2) 1 yr earlier and had achieved complete remission of the disease after chemotherapy. While awaiting allogeneic bone marrow transplantation, he underwent MRI of the brain, which illustrated a homogeneously enhancing mass occupying almost the entire temporal bone. The meninges of the fusiform gyrus in the temporal lobe, near the mass, showed pachymeningeal enhancement, strongly suggesting intracranial invasion of the mass. Bone marrow biopsy revealed a relapse of the leukemia. Re-induction chemotherapy was initiated and after the first cycle of chemotherapy the leukemia remitted and the size of the my eloid sarcoma decreased rapidly. The patient received another 3 cycles of chemotherapy, and intrathecal chemotherapy once. Follow-up brain MRI showed a tiny, non-enhancing mass at the mastoid, and we concluded that the myeloid sarcoma had disappeared. He subsequently underwent allogeneic bone marrow transplantation and, at this writing, is alive without experiencing any further problems.
Case 4
A 16-yr-old male presented with right-side otalgia and fullness of both ears. He had been diagnosed with a relapse of AML (M2) 5 months earlier for which he underwent chemotherapy, but his bone marrow showed incomplete disease remission. The right tympanic membrane appeared to be inflamed and the left one turbid. Pure-tone audiometry showed a bilateral conductive hearing loss of 20 dB. The patient was prescribed antibiotics empirically for the otitis media, but the symptoms and middle-ear effusion did not resolve after 1 month of conservative treatment. MRI of the temporal bone was conducted to determine whether a lesion was causing the middle-ear effusion. T1-weighted post-contrast images showed a heterogeneously enhancing mass invading the clivus and both petrous apexes, mastoid cavities, and middle ears. Secondary otitis media was thought to be due to the mass. Since the patient already had a history of relapsed leukemia and his general condition was very poor, the mass was not biopsied and was regarded as myeloid sarcoma. Despite treatment with additional craniocephalic radiotherapy, the myeloid sarcoma did not decrease in size. He died of pulmonary hemorrhage asphyxia 2 months later.
Case 5
A 15-yr-old female previously diagnosed with AML (M2) presented with bilateral otalgia during the course of re-induction chemotherapy. Remission of the leukemia was not achieved following induction chemotherapy. The right tympanic membrane was amber-colored and the left tympanic membrane inflamed. She was diagnosed with acute otitis media and treated accordingly. After 1 month of conservative treatment, the patient presented with mild autophonia on the right side. However, both tympanic membranes were normal and pure-tone audiometry showed no abnormality. Her leukemia was still refractory to re-induction chemotherapy, but her general condition did not worsen. Four months later, she presented with intractable headache that did not respond to analgesics. Brain MRI showed a huge mass on the sphenoid clivus that invaded the left petrous apex, while enclosing the internal auditory canal, the left occipital condyle, sphenoid sinus, ethmoid sinus, and nasopharyngeal mucosa. Based on the patient's clinical history, the mass was presumed to be myeloid sarcoma. To relieve her symptoms, brain radiotherapy was carried out but she expired due to exacerbation of the leukemia.
DISCUSSION
Ear involvement has been described in chronic and in acute leukemia. Berlinger (3) reported that leukemic infiltration of the middle-ear cleft occurs in one-third of patients and tends to follow the mucosal folds to the ossicles and intratympanic muscles, and into the tympanic membrane. Among 45 temporal bones from 25 leukemic patients, Paparella et al. (4) reported that 7 patients (28%) had experienced clinical problems for which a leukemic etiology could not be established, but 5 patients (20%) had otologic complications directly attributable to the leukemia. Not only malignant infiltrates but also hemorrhages and infections of the middle and inner ear result in otologic symptoms (1, 2). Biochemical changes affecting the sensitive structure of the inner ear, such as vascular permeability changes or alterations in the ion concentrations between the endolymph and perilymph, may also lead to symptoms (1). Very rarely, otologic symptoms result from myeloid sarcoma.
Myeloid sarcoma is characterized by the occurrence of one or more tumor masses consisting of immature myeloid cells and presenting at an extramedullary site (5). It may develop de novo or concurrently with AML, myeloproliferative disorder, or myelodysplastic syndrome (5). The true incidence of myeloid sarcoma is not known (6) and, because of its rarity, large-scale studies are lacking. Recently, Pireli et al. (5) reported the characteristics of myeloid sarcoma in an analysis of 92 patients. The commonest sites were skin (28.2%), lymph node (16.3%), testis (6.5%), and intestine (6.5%). Bone involvement accounted for 3.25% of the cases. Thus, myeloid sarcoma involving the temporal bone is very rarely seen in clinical practice.
Myeloid sarcoma is considered to be part of a systemic malignancy. In this context, a comparison between the clinical features of our five cases with those of metastatic lesions of the temporal bone is justified, and will further our understanding of the unique features of temporal bone myeloid sarcoma. Possible primary sources of metastatic lesions to bone and thus to the temporal bone are breast, lung, kidney, stomach, prostate, larynx, and thyroid (7). Gloria-Cruz et al. (8) analyzed 415 temporal bones from 212 patients with primary non-systemic malignant neoplasm. The most common symptom was hearing loss (40.4%), followed by vertigo (14.9%), facial palsy (14.9%), and tinnitus (12.8%); however, 36.2% of the patients were asymptomatic. In our series, 3 patients had hearing loss (60%), and 1 (20%) had facial palsy, similar to the rates in patients with metastatic lesions. Two of our patients had postauricular swelling and 1 had EAC swelling, neither of which frequently occurred in the presence of a metastatic lesion.
Myeloid sarcoma seems to involve the temporal bone more randomly and diffusely than non-systemic malignancy, as reported by Berlinger (3). However, there is a greater tendency of mastoid involvement. Four of our 5 patients (80%) had mastoid involvement, as determined radiologically. There are very few published case reports of myeloid sarcoma involving the temporal bone. Most of them involved the mastoid, and the patients presented with symptoms related to mastoid involvement (2, 4, 9-13). The predominance of the tumor in the mastoid cavity can be explained by that fact that the latter is more vulnerable to harboring a mass than the hard petrous bone.
In non-systemic malignancy, Gloria-Cruz et al. (8) reported that metastatic lesions commonly (82.9%) involved the petrous apex, with the mastoid involved in 21 cases (27.6%), usually by hematogenous spread. The authors stated that the hematogenously spreading tumor cells must first pass the petrous apex before involving the mastoid (8).
In leukemic infiltrations, Berlinger et al. (3) also reported that the marrow space of the petrous apex was almost always involved. If pathologic testing of the entire temporal bone had been possible in our patients, it might have revealed leukemic infiltration of the petrous apex; instead, there were 3 cases of radiologically confirmed petrous bone involvement.
Myeloid sarcoma is not easily diagnosed when the presenting symptoms mimic otomastoiditis, especially since leukemia patients are highly susceptible to bacterial, viral, or fungal infections (14). Two of our patients with postauricular swelling (cases 2, 3) were diagnosed easily within 1 month of their first visit to our clinic, whereas one patient with persisting middle ear effusion (case 4) was not diagnosed until 2 months, and another (case 5), whose middle-ear effusion was resolved with antibiotics, was not diagnosed until 5 months after visiting our clinic. One patient with EAC swelling (case 1) had been treated for otitis externa for 1 month before he was seen at our hospital.
Biopsy is the most preferred diagnostic method but is not always feasible. A biopsy sample may be difficult to obtain, especially when the mass is in an anatomically difficult site such as the petrous bone. Even if the mass is located in a site that is easily reached, biopsy is not feasible for patients with thrombocytopenia or acquired consumption coagulopathy (14).
Both CT scan and MRI are diagnostically very useful, but MRI better reveals the exact extent of the tumor and potential invasion of the cranial nerve or intracranial structure. Noh et al. (15) analyzed radiologic features of myeloid sarcoma in 11 patients. They concluded myeloid sarcoma is seen as homogenously enhancing and well demarcated mass with adjacent bony erosion in CT and MRI images. And they added myeloid sarcoma should be strongly considered in patients with myelogenous leukemia even if the imaging appearance is non-specific to myeloid sarcoma. We observed relatively well demarcated mass in case 3, but another 4 cases showed poorly demarcated lesion. And 3 of our cases showed homogenously enhancing pattern. Our findings are rather different from Noh's results, but we think clinical history of patient is also important to make a diagnosis.
Two of our patients were diagnosed by pathologic study, and another by an imaging study and clinical history. All of the patients, who were not diagnosed by pathologic study, showed relapsed or unresolved leukemia on bone marrow study. They presented with a mass lesion, seen radiologically, and their symptoms did not resolve with antibiotics. In the patient described in case 3, the mass was reduced by chemotherapy, thus confirming the diagnosis. But, in cases 4 and 5, the leukemia did not respond to chemotherapy and the clinical states of the patients rapidly worsened. Autopsy was not performed.
The single most important point in the diagnosis of temporal bone malignancy is suspicion. Physicians should be alert to the patient's symptoms. Maddox emphasized the symptom triad of otalgia, periauricular swelling, and facial nerve paresis as being highly suggestive of malignant involvement of the temporal bone. In addition, physicians should not overlook those symptoms that commonly accompany otomastoiditis, such as persisting effusion, when the patient has a systemic or non-systemic malignancy (1).
There is no standard treatment for myeloid sarcoma, especially when it occurs de novo (5, 6); rather, treatment is similar to that of systemic disease, as it is considered a manifestation of such. When a patient with myeloid sarcoma has leukemia or relapsed leukemia, combination chemotherapy for acute leukemia may induce complete remission. Additional craniocephalic radiation therapy is often considered when the disease persists after chemotherapy (6, 14). Systemic chemotherapy also may induce complete remission in the patient with de novo myeloid sarcoma (6, 16).
The prognosis of myeloid sarcoma is unfavorable. Pileri et al. (5) reported that of the 67 patients for whom follow-up data were available, 60 died from the disease (89.5%). Interestingly, all 7 survivors achieved complete remission of their myeloid sarcoma following first-line therapy, in contrast to only 8 of the 60 patients who died achieved complete remission. Bone marrow transplantation resulted in longer survival than conventional therapy. Based on these results, the authors strongly recommended that patients with myeloid sarcoma undergo high-dose therapies as a front-line approach, as it seems to be the only chance to achieve complete remission and to cure the disease. In our series, the patient of case 3, who only achieved complete remission after re-induction chemotherapy, was the only one to survive.
Even though the prognosis of myeloid sarcoma is very poor, it should be diagnosed as early as possible because early high-dose therapies offer the only possibility of cure. Finally, in leukemic patients, even in those in complete remission, physicians should not overlook symptoms mimicking otomastoiditis and must bear in mind the possibility of myeloid sarcoma.