|
 |
- Search
AbstractObjectivesTo investigate the correlation of objective audiometry with user satisfaction as measured with the questionnaire scores.
MethodsTwenty patients with hearing loss, who agreed to wear a hearing aid and were referred for hearing aid fitting, were included in this prospective clinical study. All patients used the in-the-canal type of Wide7 hearing aid provided by BSL Co., Ltd. We performed the Korean version of the Hearing Handicap Inventory for the Elderly (K-HHIE) and the International Outcome Inventory for Hearing Aids (K-IOI-HA) before and 1, 3, and 6 months after wearing the hearing aid. We also performed pure tone audiometry (PTA), speech audiometry (SA), functional gain (FG), hearing in noise test (HINT), and central auditory processing disorder tests, such as frequency pattern test (CA-f), duration pattern test (CA-d), and dichotic test (CA-Di). Patients were divided into two groups (group A-HHIE, improved; group B-HHIE, same or worse) by comparing the score of K-HHIE before and 6 months after wearing the hearing aid. In the 6-month K-IOI-HA questionnaire, 21 points were considered as the average score. Based on this, we further divided patients into two groups (group A-IOI, >21 points; group B-IOI, ≤21 points).
ResultsGroup A-HHIE included six patients and group B-HHIE included 14 patients. In PTA, SA, HINT, CA-d, and CA-Di, group A-HHIE showed higher improvements than group B-HHIE, which were not statistically significant. Group A-IOI included 12 patients and group B-IOI included eight patients. No statistically significant difference was noted in the improvement of audiometric results over a period of 6 months after wearing the hearing aid between groups A-IOI and B-IOI.
ConclusionThere were no significant and consistent audiometric results to reflect patient’s satisfaction with the hearing aid. Therefore, when analyzing the hearing aid-fitting outcome, both the objective audiometric tests and subjective questionnaire should be performed together for validating hearing aid performance.
Hearing impairment degrades the quality of life, resulting in poor communication, limited social activities, reduced ability to protect oneself, and even psychological depression, especially among the elderly [1,2]. A hearing aid is a crucial tool for making communication free and convenient for patients with hearing loss [3,4]. The prevalence of hearing aid use was 14.2% in the United States during 1999–2006 [5] and 12.6% in South Korea during 2010–2012 [6]. Despite the usefulness of hearing aids, the usage rate is quite low considering that hearing loss prevalence that ranges from 20% to 40% [5-7]. There are more people who acquire hearing aids, but only 60%–70% use them regularly [5,8,9]. Some studies have shown that the most commonly reported reasons for poor regular usage are factors related to hearing aid value, that is, insufficient benefit from using the hearing aid and comfort-related issues in wearing it [10-13]. These reasons include factors such as the hearing aid not being effective with poor benefit or poor sound quality in noisy environments and being unsuitable for the type of hearing loss that can be supplemented by a delicate and precise fitting process. The fitting procedure consists of audiometric testing and evaluation of users’ psychosocial performance after a specified period of hearing aid adoption [14]. In addition to pure tone audiometry (PTA), functional gain (FG), and speech audiometry (SA), several objective hearing tests are used to adjust the hearing aid for optimized benefit—auditory steady-state response; real ear measurement (REM); hearing in noise test (HINT); and central auditory processing disorder (CAPD) tests [14-17]. The Hearing Handicap Inventory for the Elderly (HHIE) and the International Outcome Inventory for Hearing Aids (IOI-HA) are globally used to assess subjective satisfaction with high reliability and validity [18,19]. To achieve successful hearing aid efficacy, it is important to confirm whether the hearing aid satisfies the patient’s needs. However, it remains unclear whether the fine results of objective audiometry can predict the patient’s satisfaction and regular hearing aid use. Brannstrom et al. [20] reported the unaided speech discrimination score (SDS) explains some of the variance in the IOI-HA global score, and Lee and Noh [21] also stated that the discrimination score is a significant predictor of successful hearing aid usage. This study aimed to determine whether objective audiometry is correlated with the user’s satisfaction, as measured with the questionnaire scores, and, if so, which objective audiometry can be used to maximize subjective satisfaction in patients with hearing aids.
This clinical prospective cohort study was performed at the Department of Otorhinolaryngology-Head and Neck Surgery at the tertiary referral hospital between November 2016 and April 2017. Hearing-impaired adult patients with PTA of 40–85 dB HL willing to wear a hearing aid were asked to participate in this prospective clinical cohort study, and 20 of the patients who agreed were referred for hearing aid fitting. Information regarding patients’ hearing loss, ages, genders, lifestyles, and audiograms were acquired. None of the patients showed neurological disorders, such as cerebrovascular disease or cognitive disorders. All the patients completed 6-month follow-up examinations. The study has been reviewed and approved by Asan Medical Center Institutional Review Board (IRB No. 2016-1140).
On the first visit, unaided hearing was evaluated using PTA and SDS. PTA was calculated as the mean of thresholds at the three frequencies (1,000, 2,000, and 4,000 Hz). Participants were provided with the ITC (in the canal)-type of hearing aid with four channels from 200 to 6,800 Hz by BSL (BSL Co., Ltd., Chuncheon, Korea). The benefit derived from the hearing aids was evaluated using PTA, SDS, FG, HINT, REM, and CAPD; the frequency pattern test (CA-f), duration pattern test (CA-d), and dichotic test (CA-Di). Fine tuning procedures were repeated 1, 3, and 6 months after wearing the hearing aid based on the patients’ feedback and audiological measurements.
Patients performed the Korean version of the HHIE (K-HHIE) and the IOI-HA before wearing the hearing aid and at 6 months after wearing the hearing aid. The K-HHIE consists of 25 questions. Patients can select from among three responses; no (1 point), sometimes (2 points) or yes (4 points). K-HHIE is composed of 25 items (12 social/situational, 13 emotional). Scores for the K-HHIE range from 0 to 100. Lower scores mean an improved hearing performance over unaided condition. The IOIHA consists of seven questions. Each question includes the following: daily use, benefit, residual activity, satisfaction, residual participation restriction, impact on others, and quality of life. Patients selects the one among the five responses. Therefore, each question can be scored from 1 to 5 points and the total score can be obtained from at least 7 to 35 points. High score indicates a positive hearing aids effect.
The patients were divided into two groups. Group A-HHIE included those with improved K-HHIE scores from the last visit, and group B-HHIE included those with the same or worse KHHIE scores based on comparing the K-HHIE scores before and after 6 months of wearing the hearing aid. According to the study of validity and reliability in Korean IOI-HA at a multicenter in Korea, the average score of the HA wearers was observed about 21 point [22]. Based on this, we divided the patients into two groups; group A-IOI included those with an A-IOI score >21 on the last visit, and group B-IOI included those with an A-IOI score of ≤21.
Age and initial audiometric results were evaluated with independent samples t-test. Repeated measures analysis of variance was used to analyze the differences in the aided objective tests scores over a period of time between the groups. In addition, the correlation between each aided audiometric result and the questionnaire score was assessed using Pearson’s correlation analysis and linear regression analysis. Data were analyzed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). A P<0.05 was considered to be statistically significant.
Twenty patients (five men; mean age, 62.5 years; age range, 37– 79 years) were included in this study. Of these, 12 patients had moderate hearing loss and eight had moderate–severe hearing loss.
The results of all hearing tests, including the K-HHIE score, suggested a significant improvement over compared to the prefitting test results, except for CA-f (Table 1). The mean K-HHIE score was 31.2 before wearing the hearing aid and 39.4 after 6 months of wearing the hearing aid, which showed a significant increase over the 1, 3, and 6 month results (P<0.05). The hearing thresholds were 60.2 dB on an average for unaided PTA, 37.8 dB for aided PTA on the first fitting, and 38.9 dB for aided PTA on the third fitting, indicating a gradual improvement (P<0.001). For the SA, the mean score of SDS was 46.4% on the first visit with an unaided setting, 78.8% of the aided SDS on the first fitting, 81.3% of the aided SDS on the second fitting, and 82.4% on the last visit, which indicates statistically significant improvement (P<0.001).
Group A-HHIE included six patients, and group B-HHIE included 14 patients. The average HHIE scores of prefitting and at 6 months after fitting, were 37.7±19.0 and 31.0±14.4 in group A-HHIE. Group B-HHIE showed the average post-fitting HHIE score of 43.0±35.5 from the prefitting score of 28.4±26.4. No statistically significant difference was noted in age and audiometric test results between the unaided groups. Group A-IOI included 12 patients, and group B-IOI included eight patients. The average IOI-HA scores of group A-IOI and group B-IOI were 27.3±4.3 and 16.1±5.3, respectively. No significant difference was noted in the prefitting measures between the two groups (Table 2).
Group A-HHIE revealed statistically significant improvement in CA-f (P=0.011). In PTA, SDS, HINT, CA-d, and CA-Di, group A-HHIE showed higher improvements than group B-HHIE, which was not statistically significant (Fig. 1). No statistically significant difference was noted in the improvement of audiometric results over a period of time between groups A-IOI and B-IOI (Fig. 2).
In the first fitting, correlation and regression analyses were performed between questionnaire score and the 11 parameters: PTA, SDS, FG (aided PTA-unaided PTA), gain of SDS (aided SDS-unaided SDS), HINT, CA-f, CA-d, CA-Di, and the number of frequencies, which real ear insertion gain (REIG) did not reach the target gain at the soft, comfortable, and loud speech levels. Only HINT demonstrated a statistically significant positive correlation with the K-HHIE score (P=0.027), while the other tests showed no statistically significant results (Supplementary Table 1). In the second fitting, eight parameters except REM were used for analysis, and only HINT showed a significant correlation with the K-HHIE score (P=0.002) (Supplementary Table 2). In the third fitting, no statistically significant results were obtained (Supplementary Table 3).
Hearing aid benefit could be assessed by comparing the aided and unaided performances measured either objectively or subjectively. The outcomes of the hearing aid-fitting process were focused on the manners to attain gains met prescribed targets for each individual. Objectively measured hearing aid outcomes have been conducted in a laboratory or clinical setting previously, which limited reflection of their listening achievement and satisfaction in real-world environments [23]. In recent years, several auditory perception tests, including HINT, sound localization test, and the CAPD test have been developed in numerous ways to provide more explicit listener auditory performances. Nevertheless, a study on the self-report outcome measures in hearing aid contended that objective measurements will never provide an adequate description of the deficits suffered by patients with hearing loss, irrespective of the procedures, materials, and numbers of auditory performance measurements [24]. This study suggested that the only practicable way to access this information was via structured questioning of the hearing-impaired person. The use of self-report measures can thus be considered useful for evaluating the subjective satisfaction of hearing aids and for obtaining hearing loss management options. Current research studies have focused on hearing aid validation, and various self-report assessments have been developed to quantify patients’ subjective benefits of wearing a hearing aid. Validation of hearing aid benefits includes assessing speech understanding, sound quality, ear balance, device comfort, overall quality of life, and the user’s perceived benefit.
Therefore, identifying the correlation between objective outcome measures and subjective satisfaction, assessed with the questionnaires, can help otologists to anticipate real-world benefits, based on laboratory findings, to modify the hearing aid fitting as required. Our study examined the correlation between objective and subjective outcome measures as a step toward validating hearing aids’ benefits. Comparison between the groups, as well as multiple linear regression analysis, could not, however, find any statistically significant association in the objective outcome measures assessed using the HHIE and IOI-HA questionnaires. Although significant correlations between HHIE and HINT scores in the first and second fittings were noted, the meaningful correlation in the third fitting was deemed invalid. Overall, objectively measured hearing aid outcomes such as PTA and SDS were improved sufficiently; however, the scores of questionnaires did not significantly improve. We think that the objective test with acoustic gain cannot measure the effect of hearing aid in everyday life, which resulted in this discrepancy between objective audiometric outcomes and subjective questionnaires. Because each individual has different pattern of life and activities, audiometric data of amplification is limited in assessing the effect of hearing aids on everyday life. For instance, even if patients with the same degree of hearing loss wear hearing aids with same gain, those who spend a lot of time in a loud and noisy place, will not be satisfied, while patients who spend a lot of time in a quiet place may have a relatively high satisfaction. In addition, other factors such as the suitability of the physical fitting of hearing aids use, feedback, or occlusion effect when worn, the presence of tinnitus and hyperacusis, should be considered in the evaluation of overall hearing aid satisfaction.
Our lack of finding a correlation between objective and subjective measures in this study coincides with previous studies. A study by Mendel [25] revealed no significant relationship between aided performance on the sentence tests and the Hearing Aid Performance Inventory (HAPI). The correlations among the various measures of objective (nonsense syllable test [NST] and HINT) and subjective (HAPI and HHIE) benefits found that the objective benefit (NST and HINT) measures were significantly correlated with one another, but not with any other outcome measures [26]. A study undertook a correlational analysis between Korean version of IOI-HA (K-IOI-HA) and each parameter (the aided PTA and aided SDS, FG) and found no significant correlations with subjective satisfaction, although they did find a difference between the target gain and REIG in speech mapping, suggesting significant negative correlations with the satisfaction scores at various speech levels [27].
Brannstrom et al. [20] evaluated each score on the separate IOI-HA items and other audiometric outcomes. There were significant positive associations with best ear SDS and the score of separate IOI-HA items in item 3 (residual activity limitation) and item 5 (residual participation restriction). The scores for each subscale on the questionnaires were not separately weighted on outcomes in our study. Moreover, their subjects had an average 2.4 years of hearing aid experience, when their IOI-HA scores were obtained. Our study, however, reported IOI-HA and K-HHIE scores obtained 1, 3, and 6 months after the last fitting. This may have affected the different outcomes. Further research is needed to investigate correlation between the scores for each questionnaire item and the audiometric variables.
The subjective satisfaction with hearing aids is affected not only by acoustic gain improvement but also by the lifestyle of an individual, including his or her personality, lifetime hearing aid experience, and the degree of activity limitation caused by hearing loss. For instance, hearing aid users who work in a noisy environment may be more troubled by the use of hearing aid. Therefore, in order to demonstrate the clinical correlation among the measures of hearing aids, further studies that involve statistical analysis of stratification of samples, including a large number of subjects, is necessary.
Audiometric results, K-HHIE, and K-IOI-HA scores after hearing aid fitting showed a statistically significant improvement over a period of time compared to those before hearing aid fitting. We compared these objective audiometric results according to the subjective questionnaire scores, but found no statistically significant differences. Better audiometric outcomes after hearing aid fitting did not always result in higher subjective satisfaction in the questionnaire. Therefore, when analyzing the hearing aid fitting outcome, both the objective audiometric tests and subjective questionnaire should be performed together as a way to validate hearing aid performance.
▪ Audiometric outcomes and subjective questionnaire scores showed a statistically significant improvement after hearing aid fitting.
▪ Subjective satisfaction in hearing aid users is affected not only by acoustic gain improvement but also by other individual factors.
▪ Objective audiometric tests and subjective questionnaire should be performed together for validating hearing aid performance.
NotesAUTHOR CONTRIBUTIONS Conceptualization: WSK, JWC. Data curation: JWP, WRC. Formal analysis: JWP. Funding acquisition: WSK, JWC. Methodology: EJH, YRH. Project administration: WSK, JWC. Visualization: JWP, MYK, WRC. Writing - original draft: MYK, WRC, WSK, JWC. Writing - review & editing: MYK, WRC, WSK, JWC. ACKNOWLEDGMENTSThis paper was supported by the Ministry of Trade, Industry and Energy (MOTIE), Korea Institute for Advancement of Technology (KIAT) in 2018 through the Encouragement Program for the Industries of Economic Cooperation Region with grant R0004488.
The authors gratefully acknowledge all participants of the research project.
SUPPLEMENTARY MATERIALSSupplementary materials can be found via https://doi.org/10.21053/ceo.2019.00871.
Supplementary Table 1.Correlation analysis between questionnaire score and variable parameters of objective audiometry on the first fitting Supplementary Table 2.Correlation analysis between questionnaire score and variable parameters of objective audiometry on the second fitting Supplementary Table 3.Correlation results between questionnaire score and variable parameters of objective audiometry on the third fitting Fig. 1.Objective audiometric test results before and 1, 3, and 6 months after wearing the hearing aid (A-HHIE, six patients; B-HHIE, 14 patients). HHIE, Hearing Handicap Inventory for the Elderly; PTA, pure tone audiometry; SDS, speech discrimination score; HINT, hearing in noise test; SNR, signal-to-noise ratio; CA-f, central auditory frequency pattern test; CA-d, central auditory duration pattern test; CA-Di, central auditory dichotic test. *Repeated measures analysis of variance. 
Fig. 2.Objective audiometric test results before and 1, 3, and 6 months after wearing the hearing aid (A-IOI, 12 patients; B-IOI, eight patients). IOI, International Outcome Inventory; PTA, pure tone audiometry; SDS, speech discrimination score; HINT, hearing in noise test; SNR, signal-to-noise ratio; CA-f, central auditory frequency pattern test; CA-d, central auditory duration pattern test; CA-Di, central auditory dichotic test. *Repeated measures analysis of variance. 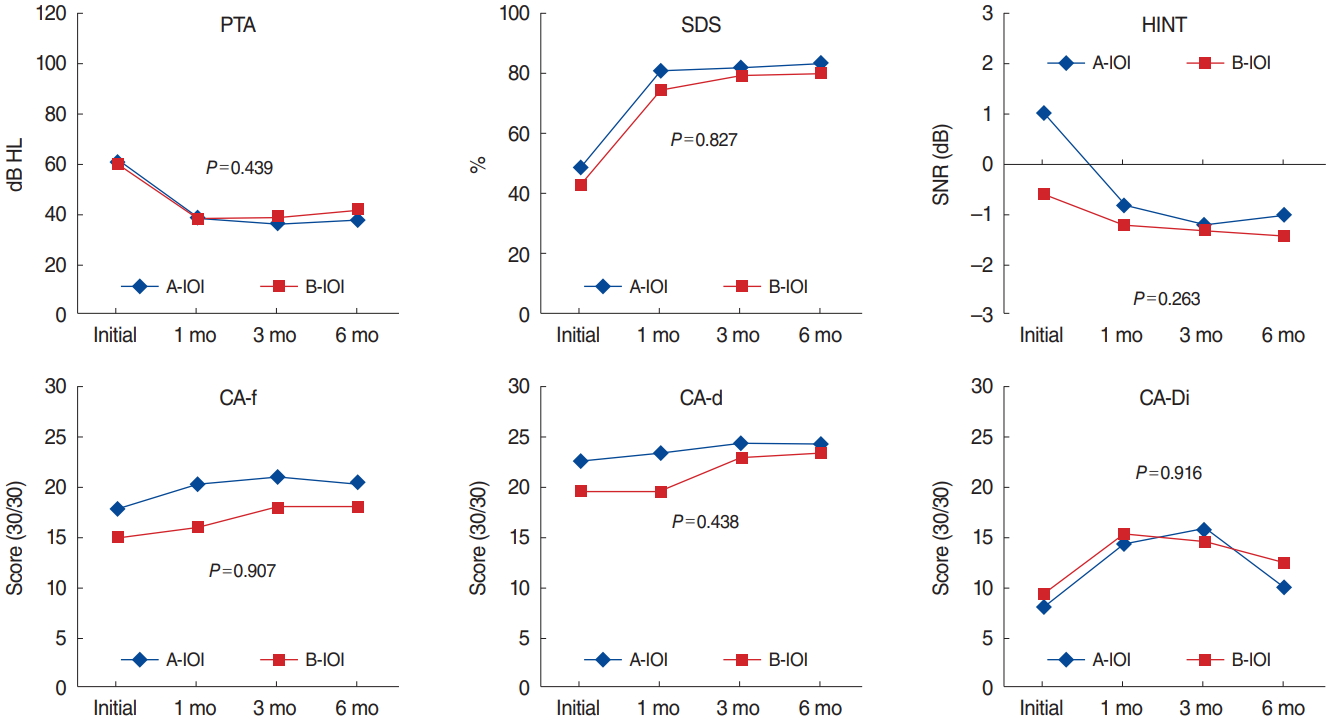
Table 1.Changes in hearing test results over 1-, 3-, and 6-month periods Values are presented as mean±standard deviation. K-HHIE, Korean version of the Hearing Handicap Inventory for the Elderly; PTA, pure tone audiometry; SDS, speech discrimination score; HINT, hearing in noise test; CA-f, central auditory frequency pattern test; CA-d, central auditory duration pattern test; CA-Di, central auditory dichotic test. Repeated measures analysis of variance (*P<0.05). Table 2.Patients’ ages and audiometry results before hearing aid fitting Values are presented as mean±standard deviation. HHIE, Hearing Handicap Inventory for the Elderly; IOI, International Outcome Inventory; PTA, pure tone audiometry; SDS, speech discrimination score; HINT, hearing in noise test; CA-f, central auditory frequency pattern test; CA-d, central auditory duration pattern test; CA-Di, central auditory dichotic test. Independent Student t-test (*P<0.05). REFERENCES1. Schoevers RA, Beekman AT, Deeg DJ, Geerlings MI, Jonker C, Van Tilburg W. Risk factors for depression in later life; results of a prospective community based study (AMSTEL). J Affect Disord. 2000 Aug;59(2):127-37.
2. Gopinath B, Hickson L, Schneider J, McMahon CM, Burlutsky G, Leeder SR, et al. Hearing-impaired adults are at increased risk of experiencing emotional distress and social engagement restrictions five years later. Age Ageing. 2012 Sep;41(5):618-23.
3. Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, Charlip WS, et al. Quality-of-life changes and hearing impairment: a randomized trial. Ann Intern Med. 1990 Aug;113(3):188-94.
4. Weinstein BE. Treatment efficacy: hearing aids in the management of hearing loss in adults. J Speech Hear Res. 1996 Oct;39(5):S37-45.
5. Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. 2012 Feb;172(3):292-3.
6. Moon IJ, Baek SY, Cho YS. Hearing aid use and associated factors in South Korea. Medicine (Baltimore). 2015 Oct;94(42):e1580.
7. Roth TN, Hanebuth D, Probst R. Prevalence of age-related hearing loss in Europe: a review. Eur Arch Otorhinolaryngol. 2011 Aug;268(8):1101-7.
8. Kahveci OK, Miman MC, Okur E, Aycicek A, Sevinc S, Altuntas A. Hearing aid use and patient satisfaction. Kulak Burun Bogaz Ihtis Derg. 2011 May-Jun;21(3):117-21.
9. Smeeth L, Fletcher AE, Ng ES, Stirling S, Nunes M, Breeze E, et al. Reduced hearing, ownership, and use of hearing aids in elderly people in the UK--the MRC Trial of the Assessment and Management of Older People in the Community: a cross-sectional survey. Lancet. 2002 Apr;359(9316):1466-70.
10. Bertoli S, Staehelin K, Zemp E, Schindler C, Bodmer D, Probst R. Survey on hearing aid use and satisfaction in Switzerland and their determinants. Int J Audiol. 2009 Apr;48(4):183-95.
11. Gianopoulos I, Stephens D, Davis A. Follow up of people fitted with hearing aids after adult hearing screening: the need for support after fitting. BMJ. 2002 Aug;325(7362):471.
12. Hartley D, Rochtchina E, Newall P, Golding M, Mitchell P. Use of hearing AIDS and assistive listening devices in an older Australian population. J Am Acad Audiol. 2010 Nov-Dec;21(10):642-53.
13. McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them. Int J Audiol. 2013 May;52(5):360-8.
14. Oh SH, Lee J. General framework of hearing aid fitting management. J Audiol Otol. 2016 Apr;20(1):1-7.
15. Sardari S, Jafari Z, Haghani H, Talebi H. Hearing aid validation based on 40 Hz auditory steady-state response thresholds. Hear Res. 2015 Dec;330(Pt A):134-41.
16. Wu YH, Bentler RA. Clinical measures of hearing aid directivity: assumption, accuracy, and reliability. Ear Hear. 2012 Jan-Feb;33(1):44-56.
17. Gil D, Iorio MC. Formal auditory training in adult hearing aid users. Clinics (Sao Paulo). 2010 Feb;65(2):165-74.
18. Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 1982 May-Jun;3(3):128-34.
19. Cox RM, Alexander GC. The international outcome inventory for hearing aids (IOI-HA): psychometric properties of the English version. Int J Audiol. 2002 Jan;41(1):30-5.
20. Brannstrom KJ, Lantz J, Nielsen LH, Olsen SO. Prediction of IOI-HA scores using speech reception thresholds and speech discrimination scores in quiet. J Am Acad Audiol. 2014 Feb;25(2):154-63.
21. Lee DH, Noh H. Prediction of the use of conventional hearing aids in Korean adults with unilateral hearing impairment. Int J Audiol. 2015;54(9):613-9.
22. Chu H, Cho YS, Park SN, Byun JY, Shin JE, Han GC, et al. Standardization for a Korean adaptation of the international outcome inventory for hearing aids: study of validity and reliability. Korean J Otorhinolaryngol Head Neck Surg. 2012;55(1):20-5.
23. Cox RM, Gilmore C, Alexander GC. Comparison of two questionnaires for patient-assessed hearing aid benefit. J Am Acad Audiol. 1991 Jul;2(3):134-45.
24. Gatehouse S. Self-report outcome measures for adult hearing aid services: some uses, users, and options. Trends Amplif. 2001 Sep;5(3):91-110.
25. Mendel LL. Objective and subjective hearing aid assessment outcomes. Am J Audiol. 2007 Dec;16(2):118-29.
|
|
|||||||||||||||||||||||||||||||||||||||||||||