|
 |
- Search
AbstractObjectivesSurgical excision via a sublabial approach is considered the standard treatment for nasolabial cysts. Although transnasal marsupialization has been proposed as an alternative method, no prospective study has compared the effectiveness of these techniques. We thus compared the surgical procedure, operating time, postoperative pain, complications, and recurrence rate between the two surgical methods.
MethodsTwenty patients diagnosed with nasolabial cysts were allocated randomly into two groups according to the surgical technique. In the sublabial approach group, the cysts were excised completely using a sublabial approach, while in the transnasal marsupialization group, the cysts were marsupialized transnasally under the guidance of nasal endoscopes. The pure operating time was measured and postoperative pain was evaluated using a visual analog scale. Complications after the procedure were assessed and recurrence was determined according to the clinical symptoms and postoperative radiologic findings.
A nasolabial cyst is an uncommon lesion that occurs in the soft tissue of the midface (1, 2). Nasolabial cysts are non-odontogenic cyst and develop lateral to the midline of the maxillary lip and alar base (3). They usually present as a swelling in the nasolabial fold, causing alar nose elevation and upper lip projection (4). They may grow slowly and painlessly over several years.
Many reports hold that surgical removal through a sublabial approach is the standard treatment of nasolabial cysts (3, 5, 6). Although the surgical outcome of this method is generally successful, complications associated with the procedure include facial swelling, gingival numbness, decreased sensation of the teeth, and wound infection (4, 7). In 1999, transnasal marsupialization was proposed as an alternative treatment method, and this technique has demonstrated several benefits compared to the conventional sublabial approach (4, 8). However, no prospective study had compared these two techniques. Thus, we compared the surgical procedure, operating time, postoperative pain, complications, and recurrence rate between the two surgical methods.
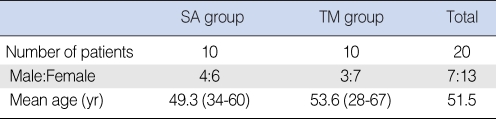
This prospective study examined patients who were diagnosed with a unilateral nasolabial cyst between January 2002 and December 2007. The diagnosis was based on the clinical presentation, anatomical location, and computed tomography (CT) findings. Twenty consecutive patients participated and were all treated by the senior author. Information on the patients is summarized in Table 1. The patients were allocated randomly into two groups according to the surgical technique. For patients in the sublabial approach group (10 cases), the cysts were excised completely through a sublabial incision, while for patients in the transnasal marsupialization group (10 cases), the cysts were marsupialized transnasally under the guidance of nasal endoscopes. Informed consent was obtained from all of the patients, and the study was approved by the Institutional Review Board.
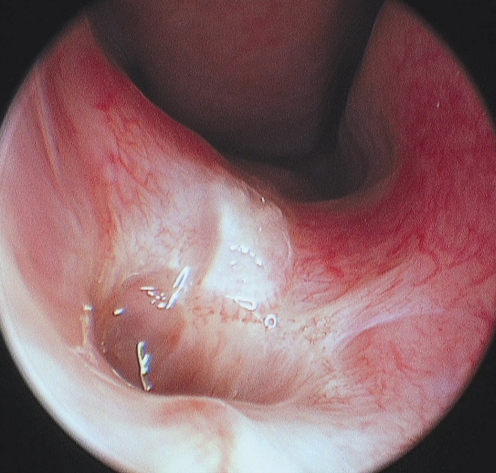
In the sublabial approach group, the surgical procedure was performed under local or general anesthesia according to the patient's preference (3 and 7 patients, respectively). First, 2% lidocaine containing 1:100,000 epinephrine was injected at the incision site. The upper gingivobuccal sulcus was incised just below the pyriform aperture, and the tissues were dissected until the smooth, well circumscribed cystic lesion was exposed. In each case, the cyst was completely extraosseous with no adhesion to the underlying bone (Fig. 1). Although the cyst was easily removed from surrounding soft tissues in some cases, tearing or rupture of the cyst occurred in other patients and part of the nasal floor mucosa was removed with the cyst because of difficult dissection between them. However, the cyst was completely removed without remnant cystic wall or epithelium in all of the cases and defect of the nasal floor mucosa was not a serious problem because the bleeding was easily controlled and the nasal mucosa rapidly healed by re-epithelialization. The incision was closed with 4.0 Vicryl (Ethicon, Somerville, NJ, USA) and a compression dressing was applied to reduce soft tissue swelling. Patients were discharged 2 days after the procedure.
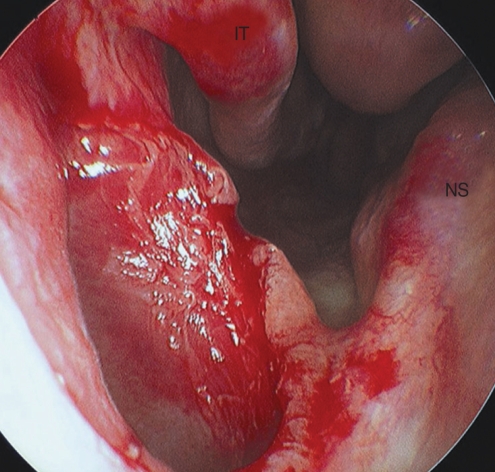
In the transnasal marsupialization group, marsupialization was carried out under local anesthesia in nine of the cases. One patient was anxious about the surgery and chose general anesthesia. The nasal cavity was anesthetized topically and decongested using cotton pledgets soaked in a solution of 2% lidocaine and 0.1% epinephrine. The anterior nasal cavity, vestibular area, and mucosal surface over the cyst were infiltrated locally with 2% lidocaine containing 1:100,000 epinephrine. An elliptical incision was made over the roof of the protruded cyst (Fig. 2). Under the guidance of rigid, straight, 4-mm diameter 0┬░ and 30┬░ nasal endoscopes (Karl Storz, Tuttlingen, Germany), the opening of the cyst was widened with a microdebrider (Medtronic Xomed, Jacksonville, FL) to at least 10├Ś10 mm in size (Fig. 3), and the cyst margins were trimmed to make smooth surface. Nasal packing was not necessary because the bleeding was easily controlled with Bosmin (Jeil Pharmaceutical Co., Seoul, Korea) gauze and the patients were discharged after several hours of observation.
The patients of each group were scheduled for follow-up once a week for 4 weeks, then the patients visited the office at 3, 6, and 12 months after the procedure. No patient was dropped out of the study during the 1-year follow-up period.
The pure operating time was measured excluding the anesthetic induction and recovery times. Patients in each group were asked about the severity of postoperative pain using a visual analog scale (VAS) in which a score of zero indicated no pain, while a score of 10 indicated extreme pain. During the follow-up period, the patients were asked whether they experienced any of the following symptoms after the procedure: cheek swelling, facial pain, facial bruising, facial tingling, facial numbness, numbness of the teeth or gingiva, and nasal bleeding. Patients with any of the symptoms were questioned further regarding the duration of symptoms. Recurrence was evaluated according to the patient symptoms and postoperative CT findings performed at 1 yr after the procedure.
The most common presenting symptom was swelling around the nose (10 patients, 50%), followed by pain (6 patients, 30%), and nasal obstruction (4 patients, 20%). When we explained the surgical technique, many patients in the sublabial approach group were fearful of the procedure and chose general anesthesia, while most of the patients in the transnasal marsupialization group agreed to local anesthesia.
The mean operating time in minutes was 46.4┬▒5.1 in the sublabial approach group and 18.3┬▒4.2 in the transnasal marsupialization group, which differed significantly (P=0.002, Mann-Whitney U-test). The VAS of postoperative pain was 6.1┬▒1.2 and 3.5┬▒0.8 in the sublabial approach and transnasal marsupialization groups, respectively (P=0.01, Mann-Whitney U-test).
During the follow-up period, eight patients in the sublabial approach group experienced one or more complications, including facial swelling, facial pain, facial bruising, and gingival and teeth numbness. Three patients in the transnasal marsupialization group had mild facial swelling. All of these complications resolved spontaneously within 4 weeks after the procedure and no permanent complications occurred. No patients had other adverse effects, including facial tingling sensation, nasal bleeding, hematoma, or wound infection.
After a 1-yr follow-up period, no patient complained of recurrent symptoms. Physical, endoscopic, and CT evaluations revealed no recurrent lesion or obstruction of the marsupialized cyst opening in either group.
Generally, excision through a sublabial approach has been accepted as the treatment of choice for nasolabial cysts (3, 5, 6). However, Su et al. (4) performed a new transnasal marsupialization method in 17 cases, which resulted in no recurrences, and other study has reported case series using this technique (2). Chen et al. (8) have recently reported microdebrider-assisted endoscopic marsupialization for the nasolabial cyst. They compared three types of surgical procedures including the sublabial approach (10 cases), conventional transnasal marsupialization (13 cases), and microdebrider-assisted marsupialization (8 cases). The surgical methods and results were similar when compared with those of our study. However, their study was conducted as a retrospective manner and no randomization was performed, which would be a limitation of the study. Although transnasal marsupialization has been reported to have advantages over the conventional approach by some authors, no prospective study had directly compared these two surgical techniques.
In terms of the surgical procedure and operating time, transnasal marsupialization was much easier and quicker than the sublabial approach because it took time to elevate the gingival flap and dissect the cyst from the surrounding structures. Bleeding control during the procedure also increased the operating time. In contrast, transnasal marsupialization required only sufficient widening of the cyst roof using a microdebrider under direct endoscopic vision, and the bleeding from the mucosal surface was controlled easily with Bosmin gauze. Moreover, most of the patients in the transnasal marsupialization group did not require hospitalization because the surgery was performed under local anesthesia in an outpatient setting.
The postoperative pain measured using the VAS was also superior in the transnasal marsupialization group. In the sublabial approach group, the mucosal incision and retraction of the upper lip during the operation could cause more pain and soft tissue swelling than transnasal marsupialization. Eight patients in the sublabial approach group also experienced one or more complications, such as facial swelling, facial pain, facial bruising, and gingival and teeth numbness. Although these side effects resolved within 4 weeks in all cases, some patients complained of great discomfort and expressed concern that the symptoms would persist permanently, especially those with numbness of the gingiva. In the transnasal marsupialization group, three patients had mild cheek swelling that resolved within 1 to 2 weeks after the procedure. In both groups, no patient experienced a recurrence of the lesion. Therefore, both the sublabial approach and transnasal marsupialization are effective methods for treating nasolabial cysts in terms of the surgical outcome.
After marsupialization, rapid epithelialization and a persistent opening were obtained because the cut edges of the nasal mucous membrane and the cyst lining were matched closely (4). However, if too small a window is made in the cyst, the annular scar surrounding the ostium will shrink rapidly and may be soon followed by mucus accumulation in the pocket or recurrence of the cyst. Therefore, a wide opening should be made to avoid recurrence (2, 4). In this study, although the size of the marsupialized cyst and opening decreased during the follow-up period in patients of the transnasal marsupialization group, no obstruction of the opening was observed in any of the patients (Fig. 4).
Histopathologically, a nasolabial cyst is a true cyst with an inner lining of ciliated respiratory epithelium (3-5, 9, 10). Marsupialization is believed to convert a nasolabial cyst into an air-containing sinus covered with ciliated respiratory epithelium similar to the mucosa of the paranasal sinuses and nasal cavity. It may act like a normal paranasal sinus with ventilation and drainage functions, resulting in the absence of mucus accumulation (4).
In our series, mucus accumulation and recurrence of the cyst, which are potential complications of transnasal marsupialization, were not observed during the follow-up period. Although both methods had successful surgical outcomes, we believe that transnasal marsupialization is a more useful procedure for the treatment of nasolabial cysts than the conventional sublabial approach because it has the benefits of a shorter operating time, no hospitalization, less postoperative pain, and low complication rate.
A limitation of our study was the small number of patients included in each group. Nasolabial cysts are relatively rare and account for only 0.7% of all maxillary and mandibular cysts (3). Since no other prospective study has compared the effectiveness of transnasal marsupialization with the conventional sublabial approach, we believe that our report has value in demonstrating the benefits of transnasal marsupialization in the random prospective manner.
Transnasal marsupialization of nasolabial cysts has many benefits over the conventional sublabial approach. It is easily and safely performed under local anesthesia in an outpatient setting. In addition, the shorter operating time, reduced postoperative pain, and low complication rate are advantages of this technique. Therefore, we propose that transnasal marsupialization be the treatment of choice for nasolabial cyst, replacing the conventional sublabial approach.
CONFLICT OF INTERESTWe do not have any conflict-of-interest or financial support with this article. References1. Lopez-Rios F, Lassaletta-Atienza L, Domingo-Carrasco C, Martinez-Tello FJ. Nasolabial cyst: report of a case with extensive apocrine change. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 10;84(4):404-406. PMID: 9347505.
2. Ramos TC, Mesquita RA, Gomez RS, Castro WH. Transnasal approach to marsupialization of the nasolabial cyst: report of 2 cases. J Oral Maxillofac Surg. 2007 6;65(6):1241-1243. PMID: 17517314.
3. Choi JH, Cho JH, Kang HJ, Chae SW, Lee SH, Hwang SJ, et al. Nasolabial cyst: a retrospective analysis of 18 cases. Ear Nose Throat J. 2002 2;81(2):94-96. PMID: 11868481.
4. Su CY, Chien CY, Hwang CF. A new transnasal approach to endoscopic marsupialization of the nasolabial cyst. Laryngoscope. 1999 7;109(7 Pt 1):1116-1118. PMID: 10401852.
5. Yuen HW, Julian CY, Samuel CL. Nasolabial cysts: clinical features, diagnosis, and treatment. Br J Oral Maxillofac Surg. 2007 6;45(4):293-297. PMID: 17030357.
6. Vasconcelos RF, Souza PE, Mesquita RA. Retrospective analysis of 15 cases of nasolabial cyst. Quintessence Int. 1999 9;30(9):629-632. PMID: 10765869.
7. David VC, O'Connell JE. Nasolabial cyst. Clin Otolaryngol Allied Sci. 1986 2;11(1):5-8. PMID: 3516463.
8. Chen CN, Su CY, Lin HC, Hwang CF. Microdebrider-assisted endoscopic marsupialization for the nasolabial cyst: comparisons between sublabial and transnasal approaches. Am J Rhinol Allergy. 2009;MarŌĆōApr;23(2):232-236. PMID: 19401056.
9. Cohen MA, Hertzanu Y. Huge growth potential of the nasolabial cyst. Oral Surg Oral Med Oral Pathol. 1985 5;59(5):441-445. PMID: 3859802.
10. Allard RH. Nasolabial cyst. Review of the literature and report of 7 cases. Int J Oral Surg. 1982 12;11(6):351-359. PMID: 6820007.
Fig.┬Ā1A round, well circumscribed nasolabial cyst was dissected from the surrounding bony structure and soft tissues via the sublabial approach. 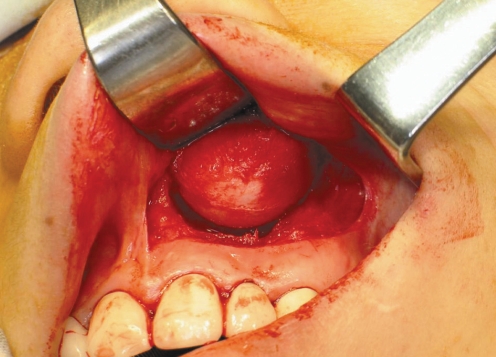
Fig.┬Ā2A protruding cystic lesion is observed on endoscopic examination of the right nasal cavity. The dotted lines indicate the elliptical incision made in the roof of the nasolabial cyst. NS: nasal septum. 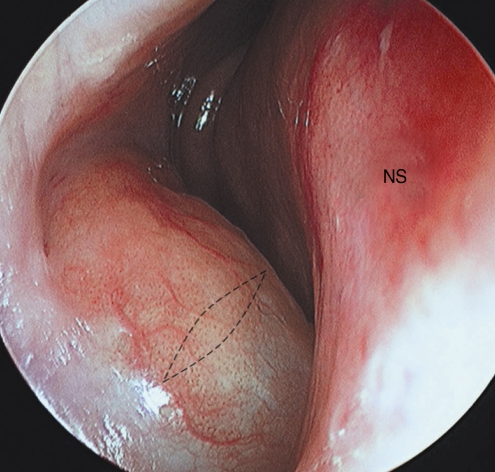
Fig.┬Ā3Endoscopic examination reveals a sufficiently marsupialized nasolabial cyst. The size of the opening exceeds 10├Ś10 mm.
IT: inferior turbinate; NS: nasal septum.
|
|
||||||||||||||||||||||||||||||||||||||