Nasopharynx as a Microbiologic Reservoir in Chronic Suppurative Otitis Media: Preliminary Study
Article information
Abstract
Objectives
The present study was designed to identify the correlations of bacterial strains of the middle ear and the nasopharynx in chronic suppurative otitis media (CSOM) patients who were scheduled for operations.
Methods
Sixty-three patients with CSOM were enrolled in the study. Culture specimens were collected from the middle ear and nasopharynx of patients who were admitted for operation. Samples collections were performed 3 times; from the middle ear and nasophaynx at the admission day, from the middle ear during the operation, and from the external auditory canal post-operatively. Bacteria were identified by gram staining and biochemical tests. The correspondence rate of organisms which simultaneously exist in the middle ear and the nasopharynx was measured.
Results
Sixty-eight organisms were isolated from the middle ear and 57 organisms from the nasopharynx among 63 patients. Of 68 bacteria identified in middle ear, 26.52% (18 bacteria) corresponded with those of nasopharynx. MRSA had the high correspondence rate, and of 18 methicillin-resistant Staphylococcus aureus (MRSA) isolated from middle ear, 33.3% (6 bacteria) corresponded with nasophaynx. Meanwhile, 3 organisms of MRSA were detected from the external auditory canal post-operatively, although they were only found in nasopharynx pre-operatively.
Conclusion
The current trend of middle ear swab alone for bacterial detection would be insufficient to identify the potent MRSA and impede early antibiotic intervention for the effective middle ear surgery. Therefore, it is necessary to perform nasopharynx cultures together with conventional middle ear culture to control potent risk for infection pre-operatively.
INTRODUCTION
Chronic suppurative otitis media (CSOM) is commonly encountered chronic inflammation of the middle ear and mastoid process, caused by dysfunction of Eustachian tube and microbacterial infections. It is important to control the acute inflammation by correct topical or oral antibiotics before the operations for favorable outcomes. But, potent bacteria and inflammation could still exist due to the alterations of bacterial strains and their antibiotic sensitivities, nosocomial infections, descending infection from mastoid or external auditory canal (EAC), and ascending infection from nasal cavity and nasopharynx.
There have been reports describing bacteriologic distributions of middle ear, mastoid and EAC in normal and CSOM patients (1-3), and some of the studies have acknowledged the value of nasopharyngeal bacterial reservoir as the etiology of acute otitis media (4-6), but there are few comparing bacteriology between nasopharynx and middle ear in CSOM patients.
The present study was designed to identify the correlations of bacterial strains of the middle ear and the nasopharynx in CSOM patients who were scheduled for operations.
MATERIALS AND METHODS
The study was performed in 63 patients, who had admitted for the CSOM operations from March to August, 2008. Their mean age was 49 years (range, 6 to 72 years), and among these patients, 26 were males and 38 were females. The patients had not been treated with antimicrobial agents for at least 2 weeks before sample collection. All were diagnosed as chronic noncholesteatomatous otitis media or cholesteatomatous otits media based on the endoscopic tympanic membrane findings and temporal bone computed tomography.
Bacteriologic sample collections were performed 3 times. At the admission day of each patient, the EAC was cleaned, and samples were collected from the middle ear through the perforation of tympanic membrane. Also, specimens from nasopharynx were obtained with cotton swab through the nasal cavity at the admission day. At the operations, samples were collected with cotton swabs from middle ear after elevating the tympanomeatal flap. And at last, post-operative specimens were obtained with cotton swab contacting the most outer surface of gelfoam in the external auditory canal on post-operation day 7.
We've collected the samples with cotton swabs while preventing contact with surrounding structures. The samples were added to Stuart transport medium and transported to the microbiology test laboratory. The swabs were plated on blood agar plate, MacConkey agar, and chocolate agar separately and the plates were incubated at 35℃ for 48 hours. Bacteria were identified by gram staining and biochemical tests. The correspondence rate of organisms which simultaneously exist in the middle ear and the nasopharynx was measured.
RESULTS
Organisms of the middle ear and the nasopharynx at the admission day
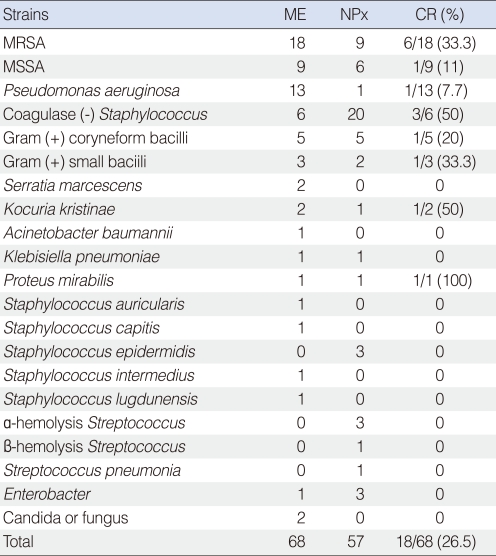
Of 63 patients who were scheduled for the operations the next day, 48 patients were culture positive in the middle ear and 38 patients were culture positive in the nasopharynx. The total numbers of organisms isolated from 63 patients were 68 in the middle ear and 57 in the nasopharynx, respectively. Of 68 bacteria isolated form the middle ear, 26.5% (18 bacteria) had the correspondence rate with nasopharynx (Table 1).
Staphylococci were most commonly found organisms in both middle ear and nasophayrnx. In the middle ear, methicillin-resistant Staphylococcus aureus (MRSA) were the most frequent isolate (26.5%) and Pseudomonas aeuginosa was the second most common bacteria. In nasopharynx, coagulase negative Staphylococcus (35.1%) was predominant, followed by MRSA (15.8%).
Culture results of MRSA
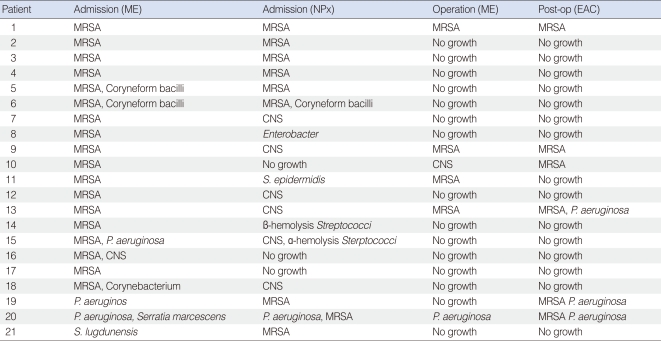
In microbiologic test conducted on the admission day, MRSA was isolated in 21 patients among 63 patients. Of 18 patients who were culture positive for MRSA in middle ear, 6 patients had MRSA simultaneously in nasopharynx (Table 2). The correspondence rate of MRSA between the middle ear and the nasopharynx was 33.3% (Table 1), relatively higher than that of other organisms.
In three patients who had MRSA only in nasopharynx and not in middle ear at the admission day, MRSA was isolated from EAC post-operatively (Table 2), although MRSA was not detected at first visits or during operation.
DISCUSSION
CSOM is characterized by its consistent and repetitive inflammatory condition, although exact pathophysiologic mechanisms of chronic state are not clearly established yet. Patients with these chronic conditions show increases in mucosal edema and effusion fluid, thus increasing the secretory capacity of mucosal glands. Because of mucosal edema and discharge, the narrow passage that connects the epitympanum of the middle ear and the mastoid cavity is blocked, and normal ventilation becomes impossible. Also, the mucosal changes reduce blood flow, resulting in alterations of bacterial strains (7). Moreover, repeat empirical prescription of antibiotics over a long period due to repeated active inflammation can possibly induce multidrug-resistant strains.
In Korea, recent bacteriological survey indicate that most commonly found organism in CSOM is S. aureus, with a prevalence of about 50%, and that 70% of S. aureus strains have been MRSA since mid-1990s (8, 9). In our study, S. aureus and P. aeuginosa were the top two most common bacteria which was consistent with the previous report (10). Also, MRSA was one of most frequent isolate (26.5%). The first strains of MRSA were identified in 1961 (11), but the proportion of nosocomial strains of MRSA has increased worldwide from 2% in 1974 to 50% in 1997 (12).
MRSA strains usually require treatment with intravenous vancomycin, which has disadvantages such as longer hospitalization, increased costs and increased risk of complications. Also MRSA infection is known to increase post-operative complication and revision operation rate, and influence the result of hearing improvement and tympanic membrane graft success rate (13). In our study, large number of patient showed pre-operative MRSA. In order to decrease and prevent the post-operative complications, the patients with MRSA were recommended to admit 2 days earlier and to receive IV vancomycin. If MRSA is identified before the surgery, physicians could prepare for the surgical outcomes by explaining to patients and administrating vancomycin earlier. However, if MRSA is isolated from cultures during or after the operation, an unexpected organism could affect the surgical results and might be considered as a source of nosocomial infection.
Palva and Hallstrom (14) in their bacteriological study of CSOM, concluded that organisms from the middle-ear pre-operatively, from the mastoid or antral tissue intraoperatively or from the canal post-operatively were identical if there was an open communication between the mastoid and middle ear. However, there are studies reporting that, although aditus was obstructed, the possibility of detecting organisms from the mastoid granulation approximates up to 60% (1). From the results of these previous studies, it is suggested that we could expect to identify same organisms from mastoid when cultures from middle ear mucosa was positive pre-operatively. Likewise, we could detect MRSA from mastoid when the aditus patency has been obtained during operations although no organisms were identified in the EAC or the middle ear pre-operatively. However, there are possibilities that the communications between the middle ear and the nasopharynx through Eustachian tube might induce MRSA infections, other than predicted potent mastoid pathogens or from nosocomial infections. In fact, there are few studies reporting the relations between nasopharynx and CSOM.
Normal bacterial flora of nasopharynx is composed of numerous coexisting strains such as Group A beta hemolytic streptococcus, S. pneumoniae, Haemophilus influenzae, Neisseria menengitidis, Moraxella catarrhalis, and S. aureu (15). Although the percentage of MRSA in nasopharynx is not established yet, the rates of S. aureus and MRSA in nasal cavity were reported as 36.4% and 9.2%, respectively (16). Moreover, the rate of MRSA colonizations in nasal cavity has increased in recent years, indicating the possible role of MRSA as the potent pathogen (17).
Of the total 21 patients in whom MRSA was isolated (Table 2), MRSA was found only in nasopharynx pre-operatively in 3 patients. However, post-operative EAC culture for MRSA was positive in these patients. The predicted pathways for the colonization of MRSA in nasopharynx are as follows. First, the infection in the middle ear might spread to the nasophaynx through descending route. Second, the repetitive refluxes of MRSA from the nasopharynx to the middle ear, an ascending route, would promote the infection in nasopharyngeal MRSA carriers and it would be relevant explanation for these patients. The current trend of middle ear swab alone for specimen collection would be insufficient to detect the potent MRSA and impede early antibiotic intervention for the effective middle ear surgery. Moreover, it is appropriate to consider both ascending and desceding routes, even in the patients who had MRSA pre-operatively in the middle ear and the nasopharynx simultaneously.
In conclusions, Staphylococci were most commonly found organisms in both middle ear and nasophayrnx, and MRSA had a relatively high correspondence rate between the middle ear and the nasopharynx. Moreover, an ascending infection from the nasopharynx to the middle ear could take place when MRSA has been isolated from the nasopharynx pre-operatively. Therefore, it is necessary to perform pre-operative nasopharynx cultures together with conventional middle ear culture to control potent risk for infection pre-operatively.
Notes
No potential conflict of interest relevant to this article was reported.