Shall We Resect the Tip of Manubrium Mallei in Tympanoplasty?
Article information
Abstract
Objectives
In tympanoplasty operations if perforation is related with malleus handle, malleus handle is desepithelised. We planned this research to investigate whether the epithelial remnants remain as a result of this desepithelisation or not.
Methods
The 35 patients who were performed tympanoplasty operation were divided into two groups. In the first group which included 13 patients the tip portion of manubrium mallei were cut off without desepithelisation. In the second group which included 22 patients the tip portions of manubrium mallei were cut off after the meticulous desepithelisation. The presence of squamous epithelium was examined histopathologically on the specimens.
Results
Squamous epithelium was observed in 9 of the 13 non-desepithelised specimens and in 6 of 22 desepithelised specimens.
Conclusion
In tympanoplasty operations despite careful desepithelisation, squamous epithelial remnants may remain on the malleus handle. So the tip of manubrium mallei could be resected to prevent the future development of cholesteatoma.
INTRODUCTION
Following the introduction of tympanoplasty by Wüllstein and Zollner in the early 1950s, many surgical approaches, grafting materials and grafting techniques have been used (1). At present two basic techniques of tympanic membrane grafting are the overlay and underlay methods. No matter what technique or material we use, the malleus handle has a special importance in tympanoplasty. While many authors claim that, malleus handle has a significant factor influencing the functional outcome, in contrast some others report that the presence of the malleus handle isn't an important prognostic factor (2-5). As Graham et al. (6) reported from their histological study the relationship between the malleus handle and the tympanic membrane at the level of umbo, the lateral squamous epithelial layer and the lamina propria embraces the manubrium intimately. Nejadkazem et al.'s study (7) about the incidence of intratympanic membrane cholesteatoma in patients after tympanoplasty revealed that, insufficient separation on the squamous epithelium rests from the handle of malleus can be responsible factor in the formation of cholesteatoma.
As known, in tympanoplasty operations if perforation is related with the manubrium mallei, the manubrium mallei are desepithelised. We planned this research to investigate whether the epithelial remnants remains as the result of this desepithelisation. For this reason during tympanoplasty operations we cut off the tip part of the manubrium mallei which forms umbo (TOMM) in one group without desepithelisation and the other group after meticulous desepithelisation and investigate the specimens histopathologically for the presence of squamous epithelium remnants.
MATERIALS AND METHODS
This research was planned as a prospective blind research (the examining pathologist did not know which group the specimen belongs to) and was performed at Ankara Ataturk Training and Research Hospital ENT Clinic.
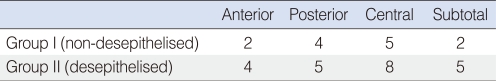
The study group consisted of 35 patients who were performed tympanoplasty operation who don't have cholesteatoma, having normal middle ear mucosa and whose tympanic membrane perforation is related with manubrium mallei. The patients who meet these criteria are chosen consequently. The 35 patients were divided into two groups. In the first group which included 13 patients, the TOMM's were cut off without desepithelisation. In the second group which included 22 patients, the TOMM's were cut off after the meticulous desepithelisation. The tympanic membrane perforations were classified as 4 groups: anterior, posterior, central, subtotal (Fig. 1). In both groups, distribution of the perforations according to this classification is shown in Table 1. All the operations were performed by the same surgeon who was the first author. All the operations were performed by post auricular approach. The edges of the perforation excised by a pick and drum remnant was desepithelised. After the elevation of tympanomeatal flap the TOMM were cut off by malleus nipper. All grafts are placed on the malleus handle while TOMM was cut off without desepithelisation at the first group which included 13 patients, it was cut off after meticulous desepithelisation by pick 90° and cup forceps at the second group which include 22 patients. To perform desepithelisation or not was decided randomly without looking the site of perforation.
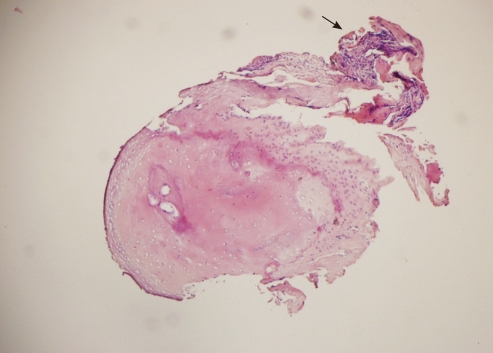
Specimens are fixed in %10 buffered formaldehyde, decalcified with %10 formic acid for 4 hours and embedded in paraffin blocks. At least 3 consecutive 4 µm-thick section levels, one of which representing the widest surface, were obtained and stained with routine hematoxylin and eosin. Slides were examined with an Olympus BX51 microscope (Olympus, Tokyo, Japan) by a pathologist, blindly. Presence of squamous epithelium was noted; even a small amount of this type of epithelium was recorded as positive.
RESULTS
The first group included 13 patients (6 male, 7 female) whose ages were between 13 and 58 (mean, 29). The second group included 22 patients (10 male, 12 female) whose ages were between 17 and 66 (mean, 38.2).
In the first group squamous epithelium were detected in the 9 of 13 samples. In the second group squamous epithelium were detected in the 6 of 22 samples (Fig. 2). In 16 samples squamous epithelium wasn't observed on the TOMM in this group.
DISCUSSION
Nowadays mainly two basic techniques such as overlay and underlay are applied for grafting of tympanic membrane. Regardless of what techniques used, in cases which the malleus handle is in close relationship with perforation, the squamous epithelium covering the malleus handle should be desepithelised. According to several authors the malleus handle has a key role in the success of the tympanoplasty and it is worthwhile to preserve it (2, 3, 5). In contrast some other authors reported that the presence of the malleus handle was not an important prognostic factor (8, 9).
According to Tos (2) the malleus handle is in contact with the drum only at the umbo and even the presence of cholesteatoma the undersurface of the malleus handle and the anterosuperior part of the drum can be visualized and keratinized squamous epithelium can be removed.
Graham et al. (6) reported in the result of their study about human tympanic membrane malleus attachment that: In the lower one third of the malleus handle (umbo) there is equal bulk of sub epithelial fibrous layer both medial and lateral to the malleus handle. In the middle third, most of the substance of the fibrous layer passes lateral to the malleus handle and the contact surface of the tympanic membrane and malleus handle is only approximately one sixth of the circumference of the malleus handle surface. According to this study and Tos (2) we can say the attachment between the tympanic membrane and malleus is most intimate at the level of umbo.
Herman et al. (10) researched the 18 long-lasting chronic otitis cases who have keratinized epithelium in the middle ear. According to them this condition, they called mallear epidermosis is characterized by: 1) a perforation of the tympanic membrane lining the handle of malleus and the umbo; 2) a proliferation of keratin surrounding the handle of the malleus and diffusing into the mesotympanum on the internal side of the tympanic membrane. In the surgical management of this entity they suggested: resection of the umbo, removal of the tympanic membrane invaded by the hyperkeratotic layers and repair by conventional myringoplasty.
Nejadhozem et al. (7) reported from their research about intratympanic membrane cholesteatoma after tympanoplasty with the underlay technique that: the most common location of these cholesteatomas is near the umbo. They concluded that: intratympanic membrane cholesteatoma after tympanoplasty may be result of insufficient removal of the residual epithelium from the handle of malleus.
In our research we found squamous epithelial remnants in 6 cases of 22 desepithelised TOMM specimens due to meticulous desepithelisation. In other words according to us it's not always possible to completely clear the squamous epithelium on the manubrium mallei. Depending on the literature findings above these squamous epithelium remnants may lead to development of cholesteatoma. In addition according to us these epithelial remnants may prevent the graft success by forming a layer between the graft and manubrium mallei. On the other hand we observed 4 squamous epithelium negative specimens in the group that the TOMM was cut off directly (without desepithelisation). In these cases the absence of the squamous epithelium may depend on desquamation due to long exposure to open air.
In this small scale study we didn't research the functional results of cutting off TOMM. For this a full scale research is required. We only wanted to emphasize that: the epithelium may remain despite careful desepithelisation. However according to us cutting of TOMM doesn't effect hearing negatively. We did not work on cholesteatoma because it develops in a long time. In our short term study occurrence of cholesteatoma is unlikely.
As a result of our research we suggest that, the TOMM could be resected in tympanoplasty in cases where the perforation is associated with the manubrium mallei and especially in cases where TOMM is close to the middle ear mucosa to prevent the development of cholesteatoma.
Notes
No potential conflict of interest relevant to this article was reported.