Fundamental Principles in Aesthetic Rhinoplasty
Article information
Abstract
This review article will highlight several fundamental principles and advances in rhinoplasty. Nasal analysis has become more sophisticated and thorough in terms of breaking down the anomaly and identifying the anatomic etiology. Performing this analysis in a systematic manner each time helps refine these skills and is a prerequisite to sound surgical planning. Dorsal augmentation with alloplastic materials continue to be used but more conservatively and often mixed with autogenous grafts. Long term outcomes have also taught us much with regards to wound healing and soft tissue contracture. This is best demonstrated with a hump reduction where the progressive pinching at the middle vault creates both aesthetic and functional problems. Correcting the twisted nose is challenging and requires a more aggressive intervention than previously thought. Both cartilage and soft tissue appear to have a degree of memory that predispose to recurrent deviations. A complete structural breakdown and destabilization may be warranted before the nose is realigned. This must be followed by careful and meticulous restabilization. Tip refinement is a common request but no single maneuver can be universally applied; multiple techniques and grafts must be within the surgeon's armamentarium.
INTRODUCTION
Primary rhinoplasty is widely performed and is often regarded as one of the more rewarding and challenging surgeries we have the privilege of performing. Many aspects of this operation give rise to the perpetual learning curve. These include the unpredictability of a single surgical maneuver, variability between patients, and the fact that the aesthetic result continues to evolve over many years. There are general principles that help guide the rhinoplasty surgeon as he/she gains experience and wisdom. This review is designed to cover broad concepts that are fundamental principles in primary aesthetic rhinoplasty.
ANALYSIS
History
The initial encounter must capture many important elements from the rhinoplasty candidate. Since one of the goals is emotional patient satisfaction, the doctor must assess some less tangible aspects of the patient. This is achieved through personal style but the end result must offer the physician a firm sense of the patient's psychological candidacy.
Perceptions and expectations
During the first visit, it is best for the environment to be warm, comfortable, private, and less sterile in appearance. It is advisable to start with open ended questioning to assess the patient's general demeanor, expectations, and perception of the physician. This is followed by more specific questioning, such as what specific features they dislike and what they would consider desirable. These questions help the surgeon and patient define expectations and goals. It is recommended that these goals be recorded and reviewed periodically as the process evolves.
Patient motivation and psychological well-being
In addition to being technically competent and a good diagnostician, the rhinoplasty surgeon must also take on the role of psychological evaluator. Personality types or social situations which raise "red flags" must be identified. Asking specific questions can help the surgeon determine the patient's motivation for the surgery. How does the patient believe this cosmetic change will affect the rest of his/her life? What kind of social support do they have? How would the patient react if their outcome was suboptimal? As difficult as it can be to discuss candidly these issues, an honest conversation about surgical outcomes and expectations is paramount in establishing trust and rapport. An aversion by the patient to discuss these topics may be indicative of an underlying psychological disorder that should be addressed.
Special considerations
The surgeon must be cautious when working with patients at the extremes of the age spectrum. Rhinoplasty is generally delayed until the age of 15 for females and 17 for males, when puberty is complete and the nasal anatomy is not expected to change or grow appreciably. These are only guidelines since minor rhinoplasties or certain functional problems may be acceptable at an earlier age. In addition, the maturity and motivation of the younger patient must be carefully assessed. Parents should be present, but some time alone with the patient can be informative in terms of assessing motivation and illicit drug use. Primary motivation should come from the patient and not the parent or through parental pressure. Moreover, social pressure as the primary motivating factor will likely be deemed "unsuccessful."
Elderly individuals seeking a rhinoplasty also represent a unique demographic. While their nasal deformity may be obvious, the patient has lived with it for their entire lives and it has become an integral part of their subconscious identity. Unlike new onset wrinkles or aging features, the nasal appearance has always been present and something they see each morning in the mirror. Altering this may impact their self image in unpredictable ways. The psychological impact of a dramatic change can be enormous and the rhinoplasty surgeon should proceed cautiously and perform only conservative changes. Anatomically, these patients may present with thinner skin, fragile nasal bones, and weakened tip support mechanisms. These abnormalities may affect the surgical approach such as performing more limited osteotomies or focusing on tip support.
Preoperative analysis
The preoperative analysis can be viewed as four stages: 1) determine what the patient dislikes about his/her nose (history), 2) perform an independent nasal analysis (physical exam), 3) identify the anatomic etiologies of the cutaneous deformities (analysis), and 4) overlap the two assessments so that patient and surgeon formulate a surgical plan. After careful analysis, the surgeon must determine if the deformity can be corrected, should be corrected, and if the correction has the potential to cause any untoward sequelae, e.g., nasal obstruction. Most importantly, the patient should leave the office with a firm understanding of what they may or may not expect from surgery.
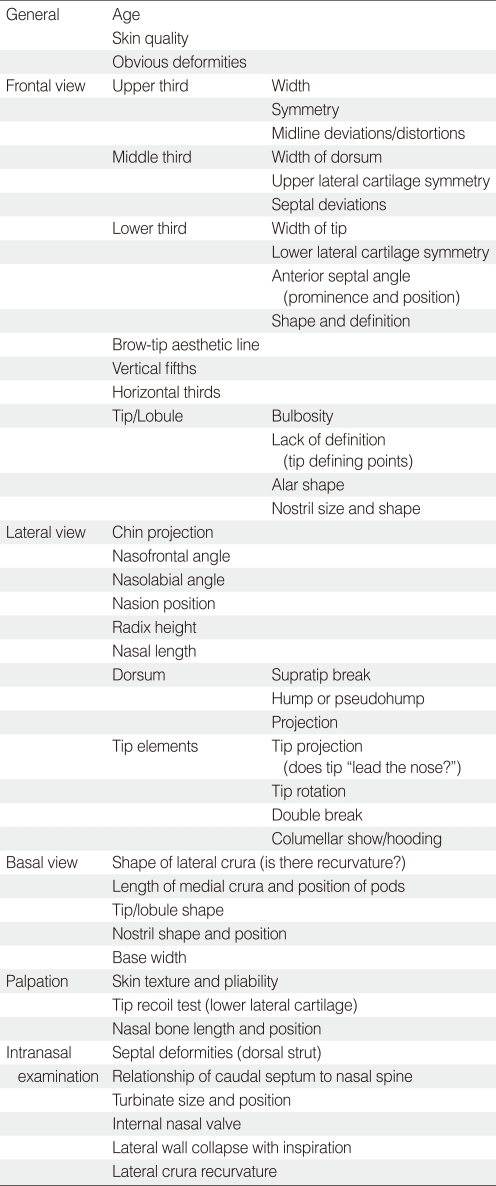
AESTHETIC ANALYSIS OF THE NOSE
Aesthetic analysis begins with universally accepted standards for "ideal" proportions, keeping in mind individual uniqueness and how those standards apply to the patient's overall facial structure. It is imperative that the surgeon analyze the entire facial structure. The goals of analysis are to define external nasal deformities, predict the underlying anatomic variations, and determine the appropriate surgical intervention. Diagnosing the underlying anatomic deformity is critical; only by addressing the deeper anatomic problem can the surgeon create the ideal surface outcome. A thorough analysis includes observation, inspection, and palpation. This should be completed in a systematic fashion with each patient so that all details are appreciated (Table 1). Performing the analysis in this manner will help avoid the "landmines" of rhinoplasty where critical anatomic variations might be overlooked.
Step 1. General analysis
Assess skin, age, and any obvious deformities (i.e., trauma or prior surgeries). The quality and thickness of the skin is important because it determines how well it will hide irregularities or drape over a new framework. Thin skin may not hide a batten graft well while thick skin may not drape appropriately over a newly refined tip framework. Remember that the skin is typically thinnest over the rhinion.
Step 2. Frontal view
Specific analysis is based on a set of defined landmarks that are itemized in Table 2. These allow effective communication and should be used accurately. In the frontal view, it is possible to assess symmetry, balance, shape, and tip contour.
Symmetry
In the frontal view, trace an imaginary vertical line in the mid-sagittal plane and assess the symmetry. Recall that many patients have some degree of underlying facial asymmetry or subtle hemifacial microsomia, and it will affect the perception of a straight nose. As an aid, one can place a straight object in the facial midline to help with defining which part of the nose is deviated and in which direction. Inspect each third of the nose independently, separating the upper, middle, and lower thirds. This will help to identify the underlying anatomic etiology for the perceived deformity. For example, when evaluating the twisted nose, asymmetry in the upper third portends bony issues. If the middle third is deviated, it is possibly due to the cartilaginous septum or upper lateral cartilage (ULC) (Fig. 1). Distortion in the lower third of the nose points to an issue with the lower lateral cartilage (LLC)'s or the anterior septal angle.
Balance
It is important to assess the overall balance of the face and how the nose fits with the person's overall facial features. Even the most perfectly formed nose will look out of place if it is too small or large for the face. Divide the face into horizontal thirds and vertical fifths to help analyze how the nose fits in proportion to the face.
Shape
The nose itself should possess an intrinsic shape and form that has aesthetic beauty and proportion. The brow-tip aesthetic line is an imaginary line traced from the medial brow down the lateral wall of the nose to the tip defining points. In the female nose the line should be slightly wider at the radix, narrow at the middle third and then widen at the tip. In the middle third, the dorsum should measure approximately 80% the width of the base. This "hourglass" shape should be subtle, unbroken, and fluid. The brow-tip line is useful for identifying irregularities at certain areas (e.g., collapse of the ULC, bony callous, or twisting of the middle vault).
Subtle convexities and concavities create highlights and shadows that are expected in the aesthetic nose. Unnatural contours can draw attention to the nose and become distracting. For example, an under-projected nose, when viewed from the front, will tend to decrease lateral wall shadowing and appear washed out across the dorsum. The brow-tip line will remain less defined. The rhinoplasty goal may be to add structure across the dorsum which would then create more natural shadowing and highlighting contours. This frees the surgeon from focusing on the shape of the individual structures and forces him/her to consider the relationship between the different aesthetic subunits.
Tip definition
The tip defining points are located at the apex of the tip lobule and formed by the junction of the medial and lateral crura of each LLC. The thickening of the cartilage in this area creates light reflection and affects perceived tip shape. Burres (1) performed an analysis of tip defining points and proposed that better defined tip points are more desirous and lead to less tip bulbosity. The lobules are bound by the alar creases, columella, and nasal bridge and should be symmetrical. Excessive alar flare is undesirable. The infratip lobule and nostril shape should be noted.
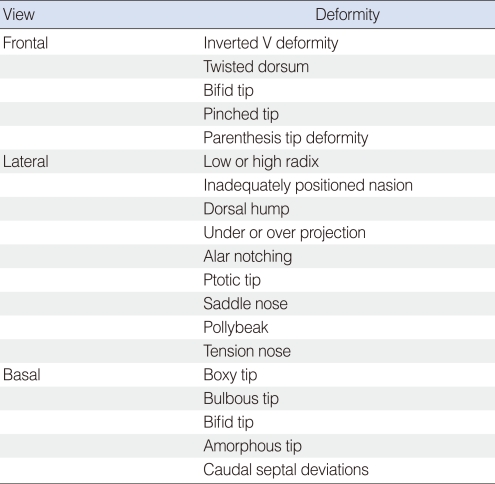
Distortions
Irregularities with shape are frequently detected on this frontal view. Deformities detected include the inverted V deformity, in which prominent nasal bones are noted above the ULC. This is usually a consequence of prior rhinoplasty due to inadequate support of the middle vault. Dorsal deviations such as a twisted, S-shaped, or C-shaped dorsum or tip deformities such as a bifid, pinched, or parenthesis tips are readily recognized in the frontal view. When dorsal deviations are noted, carefully examine the septum for deformity as well.
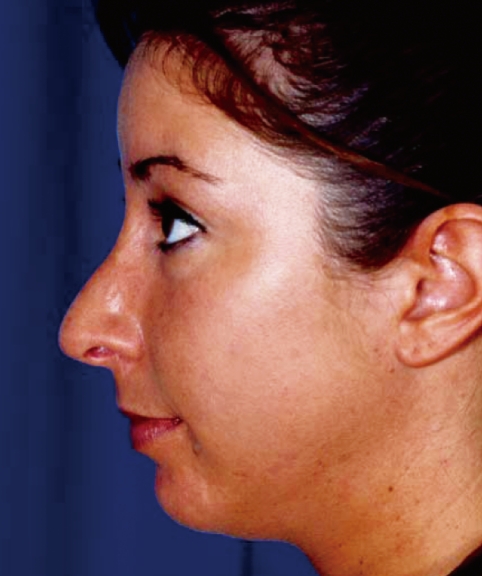
Step 3. Lateral view
The lateral view allows for determination of nasal length, projection, and rotation. In addition, distortions such as dorsal convexity/concavities or alar retraction can be noted. Important points in lateral view analysis are chin projection, nasion position, radix height, dorsal shape, tip projection, and rotation. One must remember that although many "ideal" proportions have been established in the literature, these aesthetic norms can be expected to evolve and vary over time.
Chin and glabellar projection
Chin and glabellar projection must be assessed before analyzing tip projection. An under-projected chin can create the illusion of an over-projected nose, and vice versa (Fig. 2). The easiest analysis of chin projection is Goode's method, which traces a line through the alar-facial crease perpendicular to the Frankfort horizontal line. The pogonion should approximate this line and sit slightly posterior to the lower lip.
The ideal nasofrontal angle is between 30 to 40 degrees. The deepest part of this angle is the nasion. Frontal bossing, in which the frontal bone is prominent and the glabella is displaced anteriorly, can create an acute frontal angle. This may lower the perceived starting point of the nose. Conversely, an obtuse nasofrontal angle can make the nasal length appear longer since the root of the nose appears higher or is ill-defined.
Nasion position and radix height
Overlooking a low radix can be disastrous in terms of surgical planning since it creates the illusion of a false dorsal hump and can mislead the surgeon (Fig. 3). Every effort must be made to assess the nasion and correct it accordingly. To begin, the starting point of the nose must be identified. The definition of the starting point of the nose varies in the literature. Many believe that the root should be established by non-nasal based landmarks. Others assert that the nasion, even if abnormally positioned, is what we routinely perceive as the start of the nose. Mowlavi et al. (2) surveyed 150 Caucasians regarding their opinion on ideal nasion position and nasion height (i.e., the radix). The preferred female nasion positions were at the ciliary margin of the upper lid or at the mid pupillary line. The preferred male nasion position was less specific, but at or above the mid pupillary line was most desirable. Therefore, a nasion at the level of the superior palpebral fold may place the starting point of the nose at a slightly higher than desirable position, at least at the time of that study. Definitions of standards of beauty continually evolve and the optimal nasion position is no exception. In addition, ethnic variations must be considered.
The radix is most accurately measured from the plane of the corneal surface to the nasion. According to Mowlavi et al. (2), the ideal Western radix height was at 10 mm anterior to the corneal plane for both men and women. A shallower radix was preferred over a deeper one. A deep radix will create the appearance of a short nose with a dorsal hump. A shallow radix will create a long nose with a poorly defined starting point.
Dorsal shape
The ideal dorsum is not perfectly straight but has a slight supratip break that is more pronounced in women. The appearance of a hump does not necessarily require dorsal resection. Under-projection of the tip creates a "pseudo-hump" that requires tip support or projection, not dorsal resection. As mentioned before, a low lying radix creates a pseudo-hump that is corrected by radix augmentation.
Tip projection
Tip projection refers to the distance of the nasal tip from the coronal plane of the face, independent of the dorsum and length of the nose. It is an important landmark to assess, control, and preserve. Important determinants of tip projection are the size & shape of the lower lateral cartilages, the height of the caudal cartilaginous septum, and its attachment to the medial crura. Different quantitative methods of assessing nasal tip projection have been described and are occasionally useful (3, 4). Under projection of the nasal tip can lead to a flattened appearance to the midface, the illusion of a prominent dorsal hump, and flattening of the alar base and nostrils. On the other hand, over projection of the tip can be evidenced by slit like nostrils, nasal valve obstruction, and an overall narrow nose.
Rotation and the nasolabial angle
Tip rotation parallels the degree of inclination of the naso-labial angle. The normal angles are 90 to 100 degrees for males and 100 to 105 degrees for females. Shorter people can often tolerate more tip rotation than taller individuals. It is essential for surgeons to realize that tip rotation and projection are intimately related and manipulating one will inevitably impact the other.
Tip and lobule characteristics
On the lateral view, be sure to note any excessive columellar show, hooding, or alar retraction. While a small amount of columellar show is preferred (i.e., 2-3 mm), the nostrils should be narrow ovals. One must further define excessive show as either being from alar retraction versus a hanging columella, which may be due to a prominent nasal spine, over development of the caudal septum, or large medal crura. Combinations of these are common. A double break between the meeting of the intermediate and medial crura is also desirable.
Distortions
The lateral view is essential for detecting a large spectrum of distortions. However, it must be remembered that the patient most often views their nose from the frontal or oblique positions. In addition to those mentioned above, alar notching, ptotic tip, saddle nose, pollybeak, or tension nose deformities are all evident on the lateral view.
Step 4. Basal view
The basal view shows the shape the lower lateral cartilages and the caudal septum. Assess for asymmetry, tip shape, and base width.
Shape of the lateral crura
When confronted with the basal view, the first step is to examine the shape of each lateral crus of the LLC. It is imperative to recognize recurvature of either lower lateral crus because this contributes to nasal obstruction, especially if dome binding sutures are used to correct a coexisting broad tip.
Length of the medial crura
Assess the length of each medial crus by analyzing the position of the tip defining points from the point of the subnasale. Any asymmetry of length will need to be corrected. If the medial crura are too long, the tip will appear over rotated and over projected. Normal maneuvers to derotate and deproject the tip, e.g., full transfixion incision, will not be effective since the pods will promptly come to rest on the nasal sill rather than displace posteriorly. The tip can be described by the "tripod" concept where the nasal tip is supported by the medial and lateral crura. According to this concept, shortening of the medial crura (i.e., the caudal-medial leg of the tripod) derotates and deprojects the tip.
General shape and width
Generally, the nose should be a symmetric triangle versus a trapezoid. The nostrils should be two thirds the length of the base and angulated from midline. Again, the base should be 1-2 mm inside vertical lines traced from each medial canthus.
Distortions
Several deformities are best appreciated on the basal view. These include the boxy, bulbous, bifid, or amorphous tip. Caudal septal deviations are also evident from this view.
Step 5. Palpation
Palpate the skin to determine thickness, pliability, and texture. A tip recoil test where the tip is manually deflected in caudal and cephalic directions assesses the strength and integrity of the lower lateral cartilages. The size and position of the nasal bones should be palpated. Support to the lateral nasal walls and the supra-alar crease in particular, is important to evaluate. If weak, small maneuvers to the tip cartilages will quickly create iatrogenic nasal obstruction.
After a thorough pre-operative analysis, the surgeon can describe natural features as well as irregularities from each view. Common examples of deformities that are detected from a given perspective are described in Table 3.
Step 6. Intranasal examination
The intranasal examination is integral in analyzing for preoperative factors that predispose a patient to nasal obstruction. Examine the entire length of the septum and note any deviations, deformities, fractures, perforations, or loss of integrity. Note the relationship of the caudal septum to the nasal spine. The size and position of the turbinates should be noted.
ANATOMIC ETIOLOGY
While a detailed review of nasal anatomy is beyond the scope of this chapter, it is important to identify the anatomic etiology of the cutaneous deformity that is at issue. It is only after this that one can proceed with a solid surgical plan. These skills can be improved while in the operating room. Once the nose is degloved and the framework revealed, it is an excellent opportunity to correlate the finding with the pre-operative photographs and specific irregularity. Tip asymmetry can often be broken down to intrinsic deformities at the framework level (Fig. 4).
A large and broad tip may be due to excessive skin thickness alone and removing cartilage will not only be ineffective, it will often prove counterproductive. At other times, the broad tip may be due to a wide angle at the intermediate crus, vertically oriented lateral crura, or simple lower lateral cartilage hypertrophy.
Other relatively minor tip irregularities may be readily apparent in individuals with thin skin. Examples of this include a pointy lesion at the tip that may resemble a cutaneous cyst but in fact represents a bossae at the intermediate crus.
SURGICAL PLANNING
After the analysis and identification of the anatomic etiologies of deformities, one moves forward with precise surgical planning. As the specific surgical maneuver, be it a resection, graft, or suture, is planned, one must think through the secondary effects of it as well. For each intervention, there is a primary impact that targets the leading aesthetic deformity. In addition, there are minor alterations that will occur. As an example, a cephalic trim will refine the nasal tip if the lower lateral cartilages are prominent. The secondary effects include some tip deprojection and cephalic rotation. These must be considered and anticipated.
Finally, illusions in rhinoplasty are a powerful tool yet often overlooked. There are numerous examples of how a specific change in one part of the nose will influence the balance of the nose on the entire face. A plumping graft at the nasolabial angle will not only blunt the angle but create the illusion of cephalic tip rotation. A chin implant can bring tremendous balance to the face and appear to reduce a prominent nose.
SURGICAL PROCEDURES
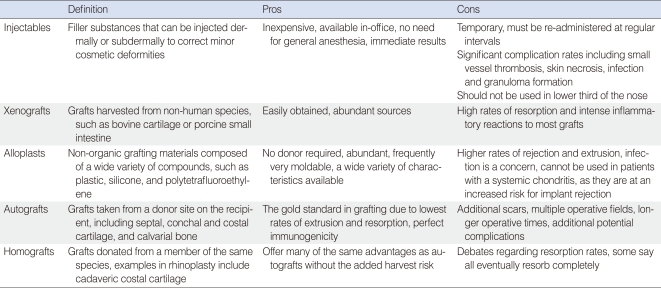
Dorsal augmentation
Augmenting the dorsum is a very common goal, especially in Asia. There are numerous techniques employed, each with their unique merits. The anatomic etiology of the low dorsum is equally varied. It may be limited to the upper third, namely the nasal bones. It can be isolated to the middle vault, the classic "saddle nose deformity." Similarly, the tip can be ptotic and require all together different techniques. Augmentation grafts can be broken down into their intrinsic material (Table 4).
Injectables
While not endorsed by many, injectable soft tissue fillers offer a less expensive, in-office alternative to surgical repair of smaller dorsal depressions. They are able to fill minor tissue defects, and are especially useful in correction of post-rhinoplasty asymmetry. The "catch" of injectable fillers is that they are temporary, must be replaced at regular intervals to maintain the aesthetic effects, and should not be used in the lower 1/3rd of the nose. Of note, this treatment method is controversial, and has been associated with small vessel thrombosis, skin necrosis, infection, and granuloma formation (5). Silicone in particular has been identified as a potential risk of necrosis, and should be carefully weighed before use. However, injectable fillers may have a more defined role in the future and the practitioner should stayed tuned with the current fillers and techniques.
Implants
North (6) first defined the ideal characteristics for an implantable material in facial reconstruction in 1953. A graft should be easily accessible, well tolerated by the host, show no tendency to perforate through skin or mucous membranes, even in areas prone to repeated minor trauma (such as the nose), and it should not show tendency to distort or resorb. Over the last century, surgeons have attempted to meet these criteria with a wide variety of materials in the face.
Xenografts
Harvested from non-human sources, these have been historically popular areas of investigation, but for the most part are not recommended for nasal reconstruction. Implantation of bovine cartilage resulted in intense inflammatory reactions and high rates of resorption (7). Some studies have explored the use of porcine small intestinal mucosa (PSIS) for nasal septal perforations with mixed results.
Alloplasts
Different substances have been tried for implantation into the body (7). Requirements include a substance that's nontoxic and nonallergenic, easy to sculpt and sterilize, and a substance that resists resorption, rejection and extrusion. These should not be used in patients with a systemic chondritis or other reactive process, as these patients will be at an increased risk for implant rejection.
1) Plastic
Tends to be well tolerated in the body, and is non immunogenic. Infection poses a serious threat to the graft, however, and can lead to extrusion. Plastics tend to be hard and immobile as well, and can shift with trauma.
2) Silicone
Silicone is the most commonly used alloplast in the nose due to its widespread use in Asia. It is a biologically inert polymer that induces a fibrous capsule around itself when implanted in the body. This capsule helps keep implants in place, which is advantageous in many parts of the body. Silicone is easy to use, can be manufactured in almost any consistency, and is easy to remove if revision is necessary. In the face, however, a significant percentage of silicone implants will shift, buckle, or extrude, and many require replacement.
3) High-density porous polyethylene
Medpor (Porex Medical, Fairburn, GA, USA) offers a highly porous, non-compressible, somewhat flexible, augmentation material that can be easily carved for nasal augmentation. The product has the ability of being malleable when submerged in hot saline (80-100℃) for several minutes, then retaining its shape permanently. The highly porous nature allows for fibrous tissue in-growth and phagocyte access to the graft, allowing for lower rates of shifting and infection respectively. The heavy in-growth of surrounding tissue can make future removal of the graft challenging.
4) Polytetrafluoroethylene
A synthetic polymer of tetrafluoroethylene, best known as its DuPont brand name Teflon, can be used to fill minor nasal soft tissue defects. A drawback of this polymer's use is that it seems to be prone to infection, and proper implantation requires meticulous handling during implantation and generous perioperative antibiotics. Long term follow up is essential to monitor future infection, rejection and fistula formation.
5) Expanded polytetrafluoroethylene (Gore-Tex)
Gor-Tex (e-Polytetrafluoroethylene; W.L. Gore Associates, Flagstaff, AZ, USA) was introduced in 1993 as a medical filler, and has provided surgeons with a pliable, natural feeling material ideal for dorsal augmentation. Gore-Tex comes in multiple thicknesses, and can be carved with a scalpel to the correct shape. Disadvantages include a possible increased risk for infection and extrusion due to the limited tissue in-growth.
Autografts
Autografts will always represent the gold standard for human implantation. Advantages include the lowest rates of extrusion and resorption, and perfect immunogenicity. Unfortunately, the use of autografts frequently requires multiple operative fields, prolonged anesthesia time, and additional scars and complications from the donor sites.
Nasal reconstruction frequently uses either autologous bone and/or cartilage. There are multiple potential donor sites, each with their own characteristics.
1) Cartilage autografts
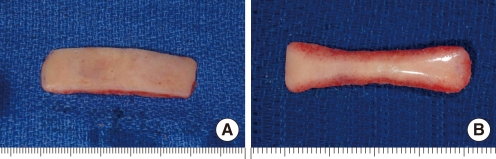
Septal cartilage: The nasal septum is a preferred site since it is in the same operative field. It is firm and flexible and can be used to provide significant structural support to the compromised nose in most patients. Unfortunately, in many saddle nose patients the quantity or quality of remaining septal cartilage is insufficient and jeopardizes further destabilization.
Conchal cartilage: Cartilage from the ear can also be safely harvested without cosmetic deformity as long as the antihelical rim is left intact. This cartilage tends to be more malleable and better suited for secondary support rather than providing a central structural foundation for the nose. Its curved shape makes it less useful for many types of caudal struts.
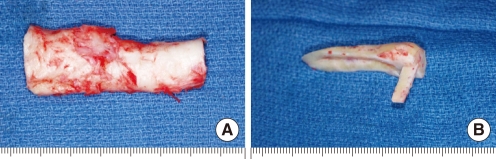
Costal cartilage: Cartilaginous ribs provide an abundant source of stiff cartilage that is utilized for many reconstructions requiring a larger graft. The structural properties of costal cartilage allow its use in larger reconstructions, and extra material can be banked in a posterior auricular pocket for future use. Harvesting does require an additional surgical field, however, as well as prolonged operative and anesthesia time. The procedure is associated with other unlikely complications, such as pneumothorax, chest deformity and post-operative pain. Cartilaginous ribs also continue to ossify, so autologous costal grafts may not be an option for cartilage in older patients. Studies suggest that when harvesting cartilage, grafts cut from the center of the rib show fewer propensities for warping than those cut from the periphery. It can be assembled into an "L" strut to provide dorsal and caudal support (Fig. 5). Bone can also be harvested from the rib if necessary.
2) Bone autografts
Bone can be harvested from the calvarium, rib, septum, or illium, and provides a rigid structure for reconstruction. It is more metabolically active than cartilage and can be prone to resorption. Bone is used less frequently than cartilage in saddle nose repair as the rigidity leaves an unnatural feel that can be problematic, especially from minor trauma. It can be used for major repair and drilled into the existing frontal or nasal bones.
Split calvarial bone: Bone grafts offer an enticing stability to an unstable deformity. They resist deformity due to contraction and scarring after reconstruction, provide good stability, and are available in abundance. Split calvarial bone has emerged as a preferred graft, with low rates of donor site morbidity, superior strength, and a lower resorption rate when compared to other sites. The dense cortex allows calvarial bone to be tapered to 1 mm and drilled to a desirable shape (Fig. 6). Drawbacks include an unnatural feel in some cases, and potential prolonged donor site pain. Central nervous system injury is rare.
Osseocartilaginous rib graft: As mentioned earlier, bone can also be harvest from rib. Some surgeons will utilize the natural osseocartilaginous junction within the graft to create a chimeric implant that replaces like with like: the bony portion overlies the nasal bones, and cartilage overlies the lower cartilaginous dorsum.
Homografts
Homografts are from another individual of the same species. Grafts are harvested from cadavers and are usually costal cartilage. They are widely abundant and do not share the same risk of donor site morbidity. If prepared correctly, they carry no risk of antigenic response (8). The antigenicity of cartilage is mediated by class II antigens that exist on the perichondrium. These can be destroyed by either removing the perichondrium or irradiating the graft with gamma radiation.
Irradiation of the graft is a method to sterilize and preserve cartilage. This has not shown to change the structural properties of the graft, such as warping, when compared to non-irradiated cartilage.
There has been debate regarding the efficacy of homologous costal cartilage grafts. The potential benefit of homografts are huge; a large donor pool allows the use of young, non-ossified costal cartilage, and the lack of a second surgical site for harvesting avoids potential surgical complications. Resorption compared to autografts is the main point of contention. Opponents of homografts state that cadaveric cartilage is rarely an acceptable option for reconstruction, citing reports of near total resorption as late as 15 years post implantation. Welling et al. (9). claimed that complete resorption of the graft should be expected, though rates of resorption remain variable. This would suggest that irradiated homografts should be contraindicated in reconstructions requiring support. Of note, many of the studied grafts were replaced by fibrous tissue, which maintained the cosmetic benefit, but did not provide the same support as cartilage. This may account for the discrepancy in patient satisfaction when these grafts are used for auricular reconstruction, where shaper margins are critical for accurate definition, in contrast to the nose where the implant serves as filler.
A recent study by Kridel et al. (8), long term advocates of homografts, describe a retrospective review of patients whom had undergone irradiated homologous costal cartilage grafting. Their follow up extended to 24 years after grafting. They evaluated 1025 IHCC grafts for warping, infection, infective and non-infective resorption, mobility and extrusion, and comparing them to autografts performed by the same surgeon. Results of the study yielded equivalent rates of warping and infection. Complication rates were much lower in patients receiving homografts (2.46% vs. 8%) due to the lack of a secondary surgical site.
Alloderm (acellular cadaveric dermal matrix) is an example of a non-cartilagenous homograft, useful in certain reconstructions. The pre-implantation treatment ablates viable cells and yields a highly biocompatible implant. Partial resorption occurs and some surgeons attempt to over-correct the deformity. Septal perforations in saddle nose deformity can be addressed with these grafts.
DORSAL HUMP REDUCTION
Reduction of the dorsal hump is a common request amongst many Western patients. There is an assumption by both patients and surgeons that this is an elementary procedure. While this task can occasionally be accomplished with much ease, there are times when serious complications can arise and lead to disgruntled patients, especially long term. Leaving too much dorsal septum at the anterior septal angle leaves a polybeak deformity that may not be apparent until all edema (including intra-operative) resolves. Future correction of this is readily performed as a "touch up" procedure.
Over resection, on the other hand, leads to more dire consequences including nasal obstruction. These serious untoward effects are best avoided by careful planning at the analysis stage. In the case of an overprojected dorsum, the pre-operative evaluation must include a careful assessment of 4 essential tenets. 1) what is the anatomy of the hump? Is it primarily bone or bone and cartilage? 2) is there a deviation to the dorsal septum, even occult and without nasal obstruction? 3) Is there a recessed chin? 4) Is the radix low?
The anatomy of the hump is important and even dictates the surgical approach we use. An over-projected hump that is exclusively bone can be reduced with osteotomies and/or rasps through an endonasal approach. A reduction of the dorsal septum will disarticulate the ULC off the septum (Fig. 7). Moreover, the new dorsal septum (after hump reduction) is narrower than the original septum which has a normal flare at the dorsal border. Continued wound contracture will lead to collapse and pinching of the ULC's and may then create an external "hour glass" deformity as well as narrowing of the internal nasal valve. With this in mind, it is imperative to anticipate this effect and repair as indicated. At the least, one should re-suspend the ULC's to the dorsal septum and for larger hump reductions, consider placing prophylactic spreader grafts to maintain middle vault width.
The hump reduction will create a new dorsal septum that will not necessarily be straight. After trimming the cartilaginous dorsum, one may unmask an occult septal deviation which leaves a twisted dorsum. This would need to be corrected accordingly.
The goal with a reduction rhinoplasty is to restore balance to the face and make the large nose less conspicuous. A small chin is an integral part of this goal and it must be specifically recognized during the pre-operative analysis. Only a few patients will be aware of this feature to their face and, if overlooked, the nose will be over-resected prior to achieving aesthetic balance. On the other hand, a chin augmentation can be powerful in terms of facial aesthetics in the setting of a large nose.
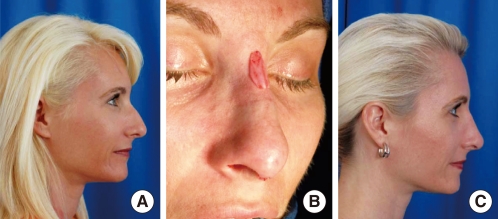
If only a few people are self aware of their small chin, even fewer will be cognizant of a low radix. A nasion that sits low on the face will create a "pseudo-hump" and resection of this dorsum can be disastrous. Instead, one should consider augmenting the radix area and raising the nasion. This may camouflage the apparent hump and allow a more conservative resection of the dorsum. The elegant nose sits in better balance on the face (Fig. 8).
TWISTED NOSE
The twisted nose is not an uncommon challenge for the rhinoplasty surgeon. Like so much of the field, successful repair begins with a careful analysis. One must specifically search out for pre-existing facial asymmetry - not uncommon in the general population. It is also important to delineate exactly which part of the nose is deviated, and in which direction. Establishing a midline reference can be useful since this part of the exam is occasionally elusive.
Deviations of the upper third are generally repaired with osteotomies. Simple medial and lateral osteotomies are not always successful because most bony deviations are post-traumatic and have a complex fracture pattern with intrinsic deformities. Traditional medial and lateral osteotomies do not necessarily cut through previous fractures. Because of this, it is often necessary to perform intermediate osteotomies which create smaller pieces of bone that can be better controlled and realigned. Additionally, a percutaneous osteotomy at the frontal beak will mobilize that triangular piece of bone that is also deviated but not freely mobile after normal osteotomies.
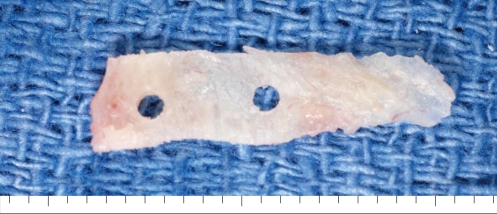
Middle vault deviations primarily involve the dorsal septum and straightening it can be one of the more challenging procedures. The algorithm for this procedure involves a progressive destabilization, realignment, followed by firm fixation and stabilization. The first step involves release of scar (in revision rhinoplasties) and the ULC's. At times, a limited dissection will permit the cartilage to straighten substantially. One then releases the mucoperichondrium on the concave side. Releasing the convex side will also help. Partial thickness scoring of the cartilage then allows immediate relief of the intrinsic "binding" forces of cartilage and will further straighten the cartilage. One usually needs to splint the corrected cartilage with either a strong piece of cartilage (as a spreader graft) or a thin piece of septal bone. Bone is effective as a splint but holes should be pre-drilled in order to avoid cracking it (Fig. 9).
More significant deviations of the caudal septum may require a complete explanatation, reorientation, and re-implantation to provide a solid dorsal and caudal "L" strut. Securing the cartilage at the dorsum is a critical move in order to prevent subsequent collapse and potential saddle nose deformity. Careful re-approximation of septal flaps and the lower lateral cartilages are essential to establish a solid platform.
TIP NARROWING/REFINEMENT
Refinement of the broad nasal tip is one of the more common goals in cosmetic rhinoplasty. Surgical options to achieve this can be categorized as:
Volume reduction
Cartilage reorientation
Augmentation
Soft tissue debulking
Choosing the appropriate technique is highly dependent on an accurate preoperative diagnosis in terms of the anatomic etiology.
Volume reduction
A resection of the cephalic portion of the lateral crura is a common technique utilized for narrowing the nasal tip. Often times this cephalic border is the culprit in tip bulbosity and its direct excision can have dramatic effects on the nasal tip. The primary effect is to narrow the supratip region and allow the tip lobule to blend in better with the upper nose. The secondary effects of such a maneuver is to create some cephalic tip rotation as well as deprojection. This technique was referred to as the "complete strip" procedure, making reference to the complete strip of cartilage left behind. Ancillary maneuvers were also performed that further narrowed the tip, such as excising triangles of cartilage from the remaining strip.
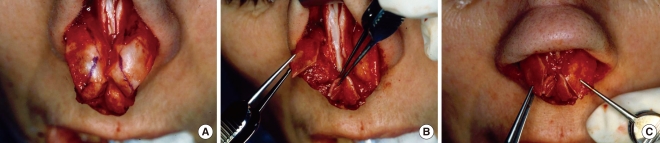
The "dead space" created by this resection led to continued contracture, collapse, and tip deformities. These stigmata include excessive columellar show due to alar retraction and nasal obstruction due to collapse of the nasal side wall and internal nasal valve. More contemporary techniques have emphasized cartilage preservation with an extremely conservatively resection of the lateral crura. The technique is better characterized as a cephalic trim rather than a resection (Fig. 10).
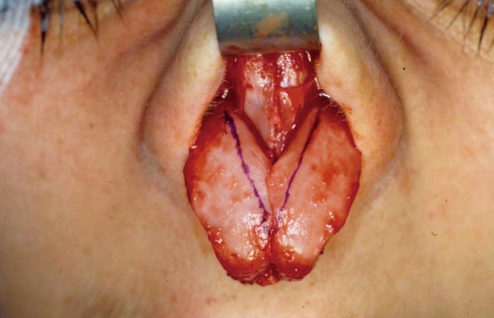
A bilateral, vertical dome division and resection of the intermediate crura is a direct method of volume reduction and narrowing the tip lobule. This technique is warranted when the boxy nasal tip is due to an excessive amount of cartilage along the intermediate crus, especially oriented in an obtuse angle. Resection in this area with primary anastomosis is an effective and direct way of correcting this problem. Cartilaginous edges are re-approximated with simple stitches and often camouflaged with a tip graft (Fig. 11).
Reorientation
A more conservative and contemporary technique for refining the nasal tip is following a concept of cartilage reorientation rather than resection. Strategic placement of sutures can change the resting orientation of the lateral crura and consequently narrow and refine the tip lobule. A broad intermediate crus can be narrowed with a "dome binding" suture placed in a horizontal mattress fashion. The suture will pinch the medial and lateral crus together, narrowing the angle between the two, and creating a more discreet tip defining point. This move will not only refine the tip but enhance projection, a powerful tool in patient with thick nasal skin (Fig. 12). One should be alerted to the recurvature of the lateral crura because the dome binding suture can pull it inward and create valve obstruction. In these cases, a "lateral crural batten graft" placed between the cartilage and vestibular mucosa will straighten the curvature and allow refinement of the tip. This can also be used when the curvature of the lateral crura is the primary cause of the tip bulbosity.
Broadly splayed tip defining points will create a wide nasal tip with a trapezoidal base. Interdomal sutures can be used to approximate the tip defining points and create a narrower and less discreet tip lobule.
Combination techniques of volume reduction and reorientation can be used for more significant deformities. The combination of a cephalic trim with dome binding sutures is a useful tandem. A vertical dome division with resection of the intermediate crura can be performed in such a way that the anastomosis will reorient the plane of the lateral crura. Excising the intermediate crus in a wedge shape with the base oriented superiorly will allow the lateral crus to reorient its plane along the lateral nasal wall. The effect of this is decreased tip bulbosity.
Augmentation
Augmentation can be an effective way of improving tip definition. The amorphous tip may be best served with a strong tip graft that protrudes beyond the existing framework and creates a new scaffold for tip support. This graft can camouflage pre-existing asymmetries, form new tip defining points, and effectively narrow the tip lobule. Tip grafts may be accurately sutured to the intermediate crura through the external approach or inserted into meticulous pockets through the endonasal route. Conventional "shield" tip grafts will support the tip, increase projection and create some derotation. More frequently, one uses a "cap" graft that is placed directly on top of the intermediate crura, thereby increasing projection and definition. This can be very effective for refining tip morphology in patients with particularly thick skin, especially ethnic noses (Fig. 13).
Soft tissue debulking
On rare occasions, it may be necessary to debulk some of the overlying soft tissue envelope in order to improve the amorphous nasal tip. This is often done in conjunction with strong augmentation grafts designed to push through the thick overlying skin. Thinning the soft tissue envelope may be needed in individuals with extremely thick skin, who paradoxically often have a poorly developed cartilaginous framework. This debulking must be done conservatively in order to avoid the subdermal vascular plexus and jeopardizing flap viability.
CONCLUSION
The field of rhinoplasty covers a wide array of surgical challenges, both in terms of technical skill and aesthetic judgment. No single maneuver can be applied to all rhinoplasty patients; only experience tells us how to pair an aesthetic goal with the appropriate technical maneuver. Any single suture or graft can have different outcomes, especially after long term follow up. Following sound fundamental principles, beginning with analysis, is the cornerstone to a successful rhinoplasty career.
Notes
No potential conflict of interest relevant to this article was reported.