Exclusively Endoscopic Resection of Nasopharyngeal Adenocarcinoma
Article information
Abstract
We reported two patients with nasopharyngeal adenocarcinoma resected by using the exclusively endoscopic approach. Case reports and a review of the world literature concerning nasopharyngeal adenocarcinoma. The tumors were resected successfully via the exclusively endoscopic approach and no conversions to the conventional approach were necessary. The two patients were followed up for 26 and 18 months respectively, and no recurrence was noted without postoperative chemotherapy or radiotherapy. To the best of our knowledge, this is the first report of endoscopic resection of nasopharyngeal adenocarcinoma. Our experience revealed that not only for the early recurrent nasopharyngeal carcinoma, the exclusively endoscopic nasopharyngectomy can be expanded for the resection of selected nasopharyngeal adenocarcinoma.
INTRODUCTION
Primary nasopharyngeal adenocarcinomas (NPACs) are extremely rare malignant tumors accounting for 0.38% to 0.48% of all malignant nasopharyngeal neoplasms and 0.70% of all nasopharyngeal carcinomas [1]. These properties mean that the treatment of choice for these tumours is total surgical resection of the primary tumor, and this has an excellent prognosis. Traditionally, because of the anatomic complexity of the nasopharynx, resection of nasopharyngeal tumors has used an external approach. However, here we suggest that an alternative exclusively endoscopic surgical strategy should be considered. This is because this tumor type is pedunculated, histologically relatively non-aggressive and, further, we have now refined our existing published endoscopic technique and successfully used it to resect different types of tumour [2-9].
Here we describe our exclusively endoscopic approach for the resection of primary nasopharyngeal adenocarcinoma. To the best of our knowledge, this is the first time to excise the nasopharyngeal adenocarcinoma via the strictly endoscopic approach. Thus, we also discuss the benefits for patients undergoing this type of operation.
CASES REPORT
The first case is a 28-year-old female with the symptoms of nasal bleeding for about 3 weeks. No neck mass was noted. Left side nasopharyngeal mass was noted by nasopharyngoscopic exam and biopsy with magnetic resonance imaging (MRI) was performed. MRI Showed an approximate 1.5 cm pedunculated nodule attaching on the left lateral wall (Fig. 1). The second case is a 58-year-old male with the symptoms of blood tinged sputum for about 1 month. No neck mass was noted. Nasopharyngeal roof mass was noted by nasopharyngoscopic exam and biopsy with MRI was performed. MRI showed an approximate 2.2 cm pedunculated nodule occupying the nasopharyngeal airway, from the nasopharyngeal roof. The pathologic biopsy report of both patients showed low-grade papillary adenocarcinoma composed of papillary fronds lined by pseudostratified columnar cells with bland unclei.
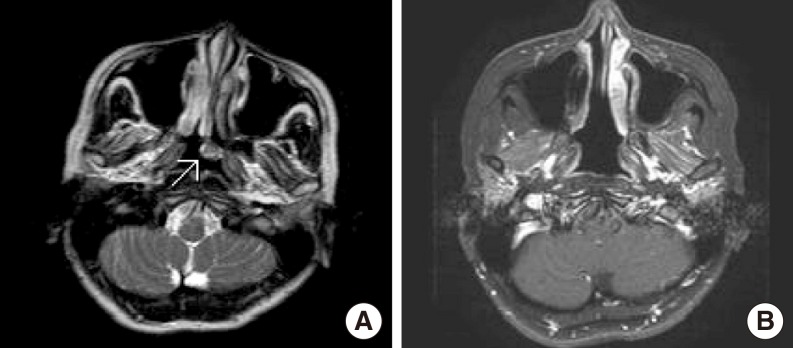
Pre- and postoperative magnetic resonance imaging (MRI) images of the patient at the level of the nasopharynx. (A) Preoperative axial MRI (T1-weighted, post gadolinium enhancement) shows the tumor (arrow) in the left nasopharynx. (B) Postoperative axial MRI (T1-weighted, post gadolinium enhancement with fat suppression) shows no detectable tumor recurrence after surgery.
According to the preoperative pathologic biopsy, we have performed 2 resections of nasopharyngeal adenocarcinomas via the exclusively endoscopic approach. The operations were performed under general anesthesia with our patient placed in a semi-sitting position. Prior to surgery, the nasal turbinates were decongested using cotton packs saturated with 1:100,000 bosmin for 15 minutes. The posterior half of the nasal septum, vomer, and inferior turbinate of the lesion site were excised to create a working space for the endoscope and to expose the tunour. Endoscope versatility has improved considerably in recent years, and by using a 4 mm diameter, 0 degree, 30 degree, and 70 degree angle endoscope (Karl-Storz, Tuttlingen, Germany), it was possible to remove the exposed tumor completely leaving an adequate mucosal surgical margin. The lateral wall of the nasal cavity (including part of the Eustachian tube), the roof (deep to the periosteum of skull base), and the posterior wall (deep to prevertebral fascia) were totally resected by a continued-wave, contact type of Diomed 25 diode laser (Diomed Co., Cambridge, UK). Frozen sections prepared from the surgical margin tissue were assessed during the nasopharyngectomy to assess whether all the tumor had been removed. The wound surface was covered with a free mucosal flap harvested from the inferior nasal turbinate and held in place by absorbable gelform. The nasal cavity was packed with nasal packing and a balloon-inflated Foley catheter for 72 hours after the operation.
RESULTS
The 2 operations were performed successfully and all surgical resection margins were free of tumor. Blood loss was minimal at only 10 mL, and no operative complications occurred. Total operation times were 100 and 90 minutes respectively, and the patients were discharged from hospital only 4 to 5 days after surgery. As the resection margins were clear there was no need to perform postoperative radiotherapy or chemotherapy. The patients were routinely followed up for 26 and 18 months respectively. No local recurrence or distant metastasis has been found to date. One of the patients' MRI pre- and postsurgery is shown in Fig. 1.
DISCUSSION
Low-grade papillary adenocarcinoma is one histologic pattern of the polymorphous low-grade adenocarcinoma. With a very low tendency for aggressive behaviour of this carcinoma, the recommended treatment of low-grade papillary adenocarcinomas is currently surgical excision, and the results are excellent [1,10,11]. Lymphatic spread been not been described in any case, so neck dissection is not normally necessary unless there is clinical evidence that suggests lymph node involvement has occurred. If it has not been possible to surgically resect all the tumor then adjuvant radiotherapy should be carried out to prevent tumor recurrence [11]. In this study, the 2 tumors were excised radically with adequate margins, thus the postoperative radiotherapy was not performed.
Nasopharynx anatomical structure is extremely complex and so existing surgical techniques use a variety of open procedures including facial translocation, midfacial degloving, maxillary swing, lateral rhinotomy, or a transpalatal approach. The surgical approach that is used depends upon both the tumor extension and the surgeon's experience and preference. In 2007, we have reported the minimally invasive endoscopic nasopharyngectomy in the treatment of recurrent T1-2a nasopharyngeal carcinoma [4]. Because of the pedunculated shape of nasopharyngeal adenocarcinomas, the relatively benign histological features of this type of tumour and also given the recent improvements in endoscopic technique and instruments [2-9], we think the exclusively endoscopic approach is feasible for selected nasopharyngeal adenocarcinoma. However, it is not the intent of this report to suggest that the exclusively endoscopic approach is superior to the conventional open approaches. Instead, the goal of this study is to highlight the experience with the minimally invasive endoscopic approach at the early juncture.
With respect to the anatomic limitations of exclusively endoscopic excision of nasopharyngeal adenocarcinoma, these would include tumor invasion to the central skull base bone superiorly, the pharyngobasilar fascia laterally, the prevertebral fascia posteriorly, and oropharynx inferiorly. It is very difficult to clarify the lateral invasion of the tumor preoperatively. If the extent of the tumor is found to be far beyond the nasopharynx during operation, we believe endosopic nasopharyngectomy can be changed to conventional open surgery without difficulty. There are still some limitations in this study. First, primary nasopharyngeal adenocarcinomas are extremely rare; we can not analyze the quality of life between our 2 cases and similar cases operated with a conventional open procedure. Second, to gain a conclusive result, we need a larger series of patients with longer follow-up. However, the early results appear encouraging.
Not only for the early recurrent nasopharyngeal carcinoma, the exclusively endoscopic nasopharyngectmy can be expanded for selected nasopharyngeal adenocarcinomas. We find that the procedure is curative, cuts down the length of the operation, decreases wound-related complications, shortens hospital stay, and moreover gives a better cosmetic outcome.
Notes
This paper was part of the lecture that was invited to present at the 3rd Asia Pacific Rhinology Innovative Leaders (APRIL) Forum on Advanced FESS and Endoscopic Skull Base Surgery, 6-8 August 2009, Hong Kong.
No potential conflict of interest relevant to this article was reported.