Partial Superficial Parotidectomy via Retroauricular Hairline Incision
Article information
Abstract
Objectives
The purpose of this study was to evaluate the usefulness of retroauricular hair line incision (RAHI) in partial superficial parotidectomy by comparison with modified Blair incision or facelift incision.
Methods
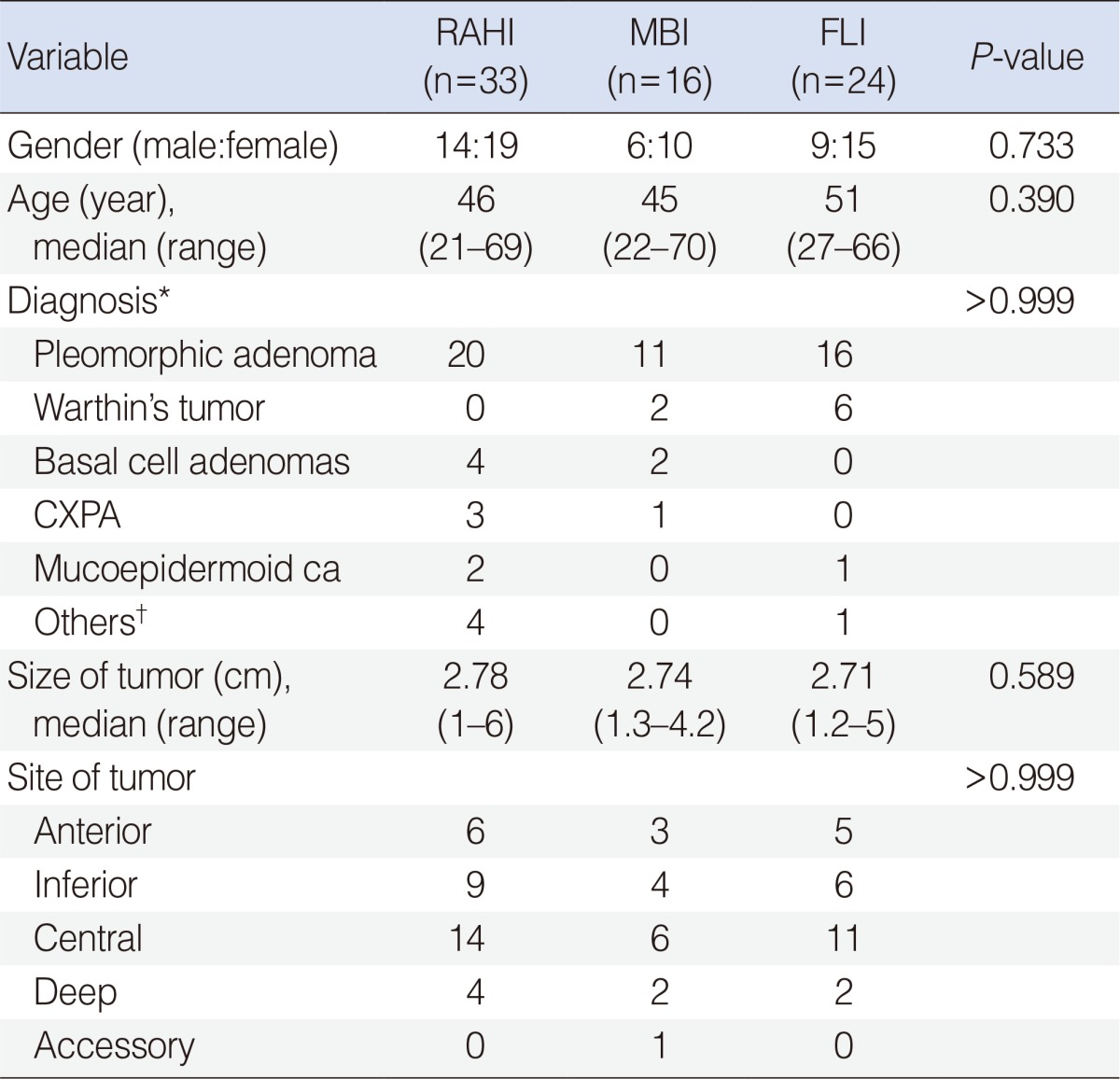
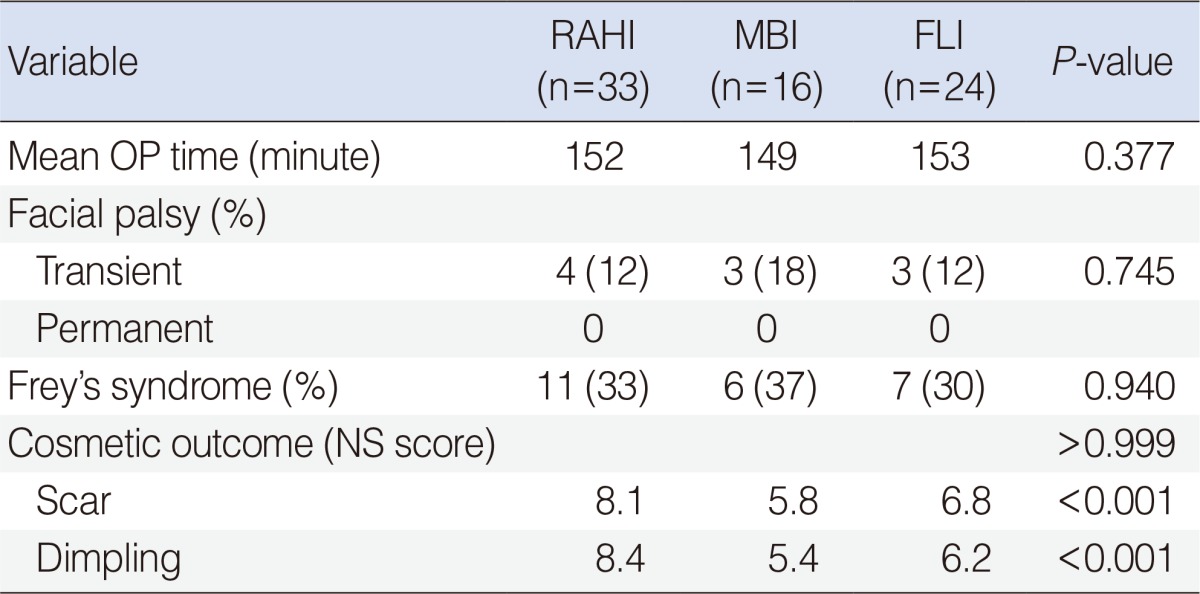
Medical records of 73 patients with benign parotid tumor who underwent partial superficial parotidectomy were retrospectively reviewed. Size and location of tumors, operative time, occurrence of facial nerve paralysis and Frey's syndrome, and cosmetic outcomes were compared among RAHI, facelift incision (FLI), modified Blair incision (MBI) groups.
Results
RAHI group showed better cosmetic results than FLI group or MBI group compared with other type of incisions (P<0.001, P<0.001, respectively). Among the 3 groups, there were no significant differences of operative time and location of tumor (P=0.377), size of tumor (P>0.999), occurrence of temporary or permanent facial nerve paralysis (P=0.745) and Frey's syndrome (P=0.940).
Conclusion
Partial superficial parotidectomy can be done safely by RAHI in most cases of benign parotid tumor. Compared with MBI or FLI, RAHI has better cosmetic outcome with no increase of operative time or postoperative complications.
INTRODUCTION
Approximately 70% of parotid tumors are accounted for by pleomorphic adenoma. Histologically, the capsule of pleomorphic adenoma is sometimes found to be missing or to be located outside of the tumor [1]. Surgical policies with regard to parotid gland neoplasm are often influenced by the preferences of the surgeon, as well as by preoperative histological finding, size of the tumor, etc. In the late 1800s, standard surgical treatment involved enucleation, but this changed to surperficial parotidectomy (SP) in the late 1900s, when histological findings indicated parotid pleomorphic adenoma [2]. However, today, most surgeons agree that the enucleation is associated with a high incidence of recurrence, while complete SP is unnecessary.
An important point in parotid surgery is preservation of the facial nerve, as iatrogenic facial palsy can be a complication. This is sometimes accompanied by further complication: postoperative hematoma, Frey's syndrome, wound defect, fistulae, sialoceles. As a result, most surgeons would prefer to preservation of the parotid during resection of benign parotid gland tumors. Recently, partial superficial parotidectomy (PSP) and extracapsular dissection (ECD) have become the norm. In PSP, the trunk of the facial nerve should first be identified as it would be in SP, but the extent of resection is limited to the tumor-bearing area of the parotid parenchyma. On the other hand, ECD relies on manipulation of the facial nerve only when it is adjacent to the tumor, and involves en bloc tumor resection while leaving the capsule intact. In a meta-analysis published in 2009, PSP seems to be superior to ECD in terms of both incidence of recurrence and persistence of facial palsy [3].
The type of incision employed during surgery of parotid neoplasm is influenced both by the preference of the surgeon and by other factors, such as the sex and age of the patient, and location of the tumor. The cosmetic implication of parotid surgery using retroauricular hair line incision (RAHI) was first published in 2009, but the report was limited to ECD [4].
The author was assumed that PSP via RAHI is more ideal. Hence, this study was designed to investigate the usefulness of RAHI in PSP, in comparison with modified Blair incision (MBI) or facelift incision (FLI), taking into account size and location of tumors, operative time, occurrence of facial nerve paralysis and Frey's syndrome, and cosmetic outcomes.
MATERIALS AND METHODS
From January 2006 to January 2011, 73 patients (44 females, 29 males) presenting with previously untreated benign parotid tumor were enrolled into this retrospective clinical study. Benign parotid tumor was assessed by fine needle aspiration and computed tomography (CT) or magnetic resonance image (MRI). Patients with benign parotid tumor underwent PSP, after being allocated to the RAHI, MBI, or FLI group for the type of incision (Fig. 1). Of the 73 patients, 22 patients underwent RAHI, 16 patients underwent MBI, and 24 patients underwent FLI. JP drain was inserted in all the patients. Drains were usually removed on the second postoperative day, at which time the amount of drainage was less than 20 mL.

Types of incsion for parotid tumor. (A) Retroauricular hair line incision. (B) Modified Blair incision. (C) Facelift incision
The site of the tumor was established from preoperative images performed by an experienced radiologist. Postoperative complications were recorded at the time of the patient's follow up visit. Cosmetic outcomes were evaluated after surgery, using an 11-point numerical scale (NS). Each patient marked the score their satisfaction about surgical dimpling and scarring, ranging from '0, not satisfied at all' to '10, most satisfied'.
The retrospective review was performed with strict discretion and confidentiality in such a way as to keep all confidential information secure and known only to the reviewers. At the time we collected our data for this study, approval was accepted by the Medical-Ethical Protocol Institutional Review Board.
The outcomes of patients who received RAHI were compared with those who received MBI or FLI, for age, sex, site of tumor, size of tumor, operative time, facial palsy, Frey's syndrome, and cosmetic results; paired t-tests were sued to compare paired samples, while χ2 test were used for analysis of categorical data. P-values<0.05 were regarded as statically significant. Data were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA).
Surgical technique
For RAHI approach, the patient's neck is extended with the help of a pillow under the upper back, and the patient's head is rotated to the opposite side, under general anesthesia. An incision is made along the postauricular sulcus and hairline, starting from the lower end of the postauricular sulcus, moving upward to the upper one-third point of the sulcus, and smoothly angled downward to continue 0.5 to 1 cm along the inside of the hairline (Fig. 2A). The incision is continued through the subcutaneous fat onto the sternocleidomastoid muscle, and the skin flap is elevated anteriorly, onto the parotid gland and the lesion site [5]. The skin flap is elevated in the plane superficial to the parotid fascia. The main trunk of facial nerve is identified by exposing the tragal pointer. The relevant branch of facial nerve is carefully dissected, allowing determination of the location and size of tumor. The tumor is removed completely, along with normal parotid parenchyma within at least 1 cm from the capsule of the tumor (Fig. 2B). After removal of the mass, the capsule and tissues of the remaining parotid gland are estimated and a suction drain is inserted, placed amongst the hair behind the lower portion of the hairline incision. The skin incision is closed securely with interrupted sutures, using 4-0 Vicryl and nylon (Fig. 2C). Drains and dressings were usually removed on the second postoperative day, at which time the patients are discharged from the hospital. In the MBI, FLI groups, surgery was done similarly to that of RAHI group except that the type of incision differed.
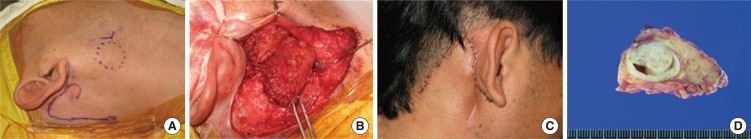
Surgical procedure of partial superficial parotidectomy via the retroauricular hair line incision approach. (A) An incision was made along the postauricular sulcus and hairline without a preauricular incision. (B) After finding the trunk of the facial nerve and its branches, partial superficial parotidectomy was performed, resulting in the removal of some surrounding parotid parenchyma. (C) Postoperative photograph of a patient, taken immediately, showing a good cosmetic outcome without a visible incision scar or a sunken defect of the parotid region. (D) The mass was removed completely, along with normal parotid parenchyma, without capsular rupture.
RESULTS
The clinical and demographic characteristics of the patients in different groups are shown in Table 1. We observed no significant differences in gender distribution, mean age, tumor size, or site of tumor between 3 groups, indicating that the location of the tumor tends not to affect the type of incision used. Table 2 shows the operation time, transient or permanent facial palsy, Frey's syndrome, satisfaction score for cosmetic results. No between-group difference was seen in operation time. In the 3 groups, the incidence of Frey's syndrome exceeded ~30%. No permanent facial palsy was seen, but a total of 11 cases of transient facial palsy were noted; all of those (100%) were of House-Brackman grade II and recovered within 3 months. There was no significant difference with respect to facial palsy between RAHI and other groups. However, as far as cosmetic results were concerned, the mean satisfaction score (0.10) for surgical dimpling and scarring was significantly higher in the RAHI group compared to the MBI and FLI groups (P<0.001, P<0.001, respectively). Other complication such as postoperative hematoma, infection, seroma or sialoceles did not occur. The median follow-up period for all these patients is 29 months (range, 4 to 52 months). No recurrence of tumor has been noted to date.
DISCUSSION
In this study, we compared the effectiveness of PSP performed using a RAHI approach. The optimal treatment for parotid pleomorphic adenoma has been a subject of considerable debate for surgeons. SP is considered a classical procedure, but it gives rise to many complications. Today, in all areas of surgery, including surgery of parotid tumors, function-preservation is emphasized [5]. Statistical analysis of published series demonstrate a significantly higher rate of recurrent pleomorphic adenoma and permanent facial nerve function with ECD compared to PSP, even though ECD is also function-preservation surgery [3,6,7]. In this respect, PSP is considered to be effective, with low postoperative complication and no tumor recurrence reported in previous studies [8,9]. In PSP, the main facial nerve trunk is first found, and the branches involved in the tumor mass are subsequently identified. ECD, in contrast, relies on manipulation of the facial nerve only when it is adjacent to the tumor, and involves a painstaking procedure performed in the plane of the tumor capsule, which must not be ruptured.
Moreover, there are a number of options with regard to the used incision for parotidectomy, with MBI being the most commonly used incision over the past 2 decades. However, retraction of the facial scar is a big disadvantage of MBI. Furthermore, in recent times, skin incision has tended towards being smaller, as long as surgical exposure is not significantly compromised, and this is particularly true for resection of benign parotid tumors. After the report by Appiani and Delfino [10], FLI has become more popular. This type of incision has the advantages of a less prominent scar and a lower likelihood of transaction of the greater auricular nerve, however, this approach still leaves a scar on the visible portion of face. RAHI was introduced as an alternative surgical approach for resection of an upper neck mass [11]. This type of incision offers a feasible procedure for the surgical management of parotid tumors. The RAHI potentially involves the least visible area of head and neck, as it is made along the postauricular sulcus and hair line. Roh [4] first used RAHI approach without a preauricular incision for parotid surgery, but, in fact, used RAHI only as the starting procedure for ECD.
Although at first it appears as if the RAHI approach can only be used in mobile benign tumors arising from the inferior superficial part of the parotid gland, our study shows that this approach can be used regardless of site or size of the tumor. Actually, our experience suggests that all tumors could be resected completely with careful dissection by RAHI approach unless the tumor was located just anterior of the external auditory canal, which creates a blind spot. Our findings also suggest that PSP via RAHI has a better cosmetic outcome compared with other type of incisions. In the 3 groups investigated in this study, there were no significant differences in operative time and location or size of tumor, or completeness of resection. Moreover, facial palsy and Frey's syndrome also did not differ between RAHI and MBI or FLI groups (Table 3).
In conclusion, PSP can be done safely by RAHI in most cases of benign parotid tumor. Compared with MBI or FLI, RAHI has better cosmetic outcome with no increase of operative time or postoperative complications. The present study needs to be validated by large-scale prospective trials with assessment for objective cosmetic results.
Notes
No potential conflict of interest relevant to this article was reported.