Results of Free Flap Reconstruction After Ablative Surgery in the Head and Neck
Article information
Abstract
Objectives
Due to the complex anatomy and function of the head and neck region, the reconstruction of ablative defects in this area is challenging. In addition, an increasing interest in improving the quality of life of patients and achieving good functional results has highlighted the importance of free flaps. The aim of this study was to summarize the results of free flap reconstruction and salvage of free flaps in a single institute, and to analyze differences in the results by the flap donor site, recipient site, and learning curve.
Methods
The medical records of patients who underwent free flap reconstruction from 2004-2012 were reviewed retrospectively. One hundred and fifty free flaps were used in 134 patients, who had an average age of 57.7 years. The types of flaps applied, primary defect sites, success rates, results of salvage operations for compromised flap, and the learning curve were analyzed.
Results
The anterolateral thigh flap was preferred for the reconstruction of head and neck defects. The overall success rate was 90.7%, with 14 cases of failure. A total of 19 salvage operations (12.7%) for compromised flap were performed, and 12 flaps (63.2%) were salvaged successfully. Dependency on the facial vessels as recipient vessels was statistically different when oral and oropharyngeal defects were compared to hypopharyngeal and laryngeal defects. The learning curve for microvascular surgery showed decrease in the failure rate after 50 cases.
Conclusion
The free flap technique is safe but involves a significant learning period and requires careful postoperative monitoring of the patient. Early intervention is important for the salvage of free flaps and for lowering the failure rate.
INTRODUCTION
Over the past decade, techniques in free tissue transfer with microvascular anastomosis have advanced and this procedure is now widely used for the reconstruction of defects following cancer ablation in the head and neck. As defects in the head and neck after tumor resection often cause significant functional and cosmetic deformity, the free flap, which can supply various kinds of tissues, is ideal for reconstruction of head and neck defects. Hence, microvascular surgery is now a very important part of head and neck surgery. If microvascular surgery is not adequately supported, head and neck ablative surgery itself cannot be performed. Therefore, providing stable support for microvascular surgery is important for the effective and timely performance of ablative head and neck surgery. Because of this, an increasing number of head and neck surgeons are choosing to perform microvascular surgery themselves.
With improvements in technique and surgical devices, the reported overall rates of success of free flaps in the literature are as high as 95% to 97% in the case of experienced surgeons [1,2,3,4]. However, failures caused by vascular thrombosis are inevitable in some cases, and this frequently leads to devastating results. Unless sufficient experience can be gained during the training period, cases of failure in the early stages of a surgeon's career are inevitable, with these experiences leading to some surgeons giving up on performing microvascular surgery early in their career.
This paper describes all of the cases of free flap reconstruction performed by a single head and neck surgeon and aims to analyze the causes of success or failure of these cases in order to illustrate the learning curve of this procedure for young surgeons starting to perform microvascular free flap surgery. In addition, this study was conducted to summarize the results of free flap reconstruction and salvage of free flaps, and to analyze the differences in results by flap donor site, recipient site, and learning curve.
MATERIALS AND METHODS
This retrospective analysis was approved by The Institutional Review Board of Seoul National University Bundang Hospital (B-1207-162-103). A retrospective chart review of 150 cases in 134 patients who had undergone free flap transfer after cancer ablation in the head and neck between May 2004 and April 2012 was performed. For each patient, data on age and sex, and anatomical location of the tumor, as well as reconstructive variables were collected. All operations were performed by a single surgeon in a single institute.
There were 100 men and 34 women in the study, ranging in age from 17 to 75 years, with an average age of 57.7 years. In all the patients, vessels were irrigated with a heparinized solution consisting of 100 units of heparin per milliliter. For the prophylaxis of thrombosis, we used intravenous prostaglandin E1 and volume expander during 5 days after surgery.
Postoperative flap monitoring was done with clinical observation and adjuncts such as pin-prick, and temperature measurements. An external skin monitor paddle for buried flaps was also used to monitor the condition of the flap. Arterial circulatory problem usually make the flap looks pale and lacks capillary refill. Otherwise, venous problem usually make the flap congested and bluish in color. For the first 72 hours, flaps were observed every 2 hours for any vascular compromise. Upon suspicion of vascular compromise, a salvage operation of free flaps was considered for re-exploration.
A salvage operation in this article was defined as an operation intended to rescue the original flap; operation with another free flap due to a failed flap was not included as a salvage operation. The term compromised flap was used to include both failed flaps and successfully salvaged flaps, in order to identify all flaps that had encountered problems. The main outcomes assessed were the types of flap used to reconstruct primary defects, success rates, flap results according to the primary defect and selected recipient vessels, results of the salvage operation, and the success or failure of the cases according to the learning curve.
The surgical outcomes were analyzed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Comparisons were based on the Fischer exact test for categorical variables. A P-value of <0.05 was accepted as significant.
RESULTS
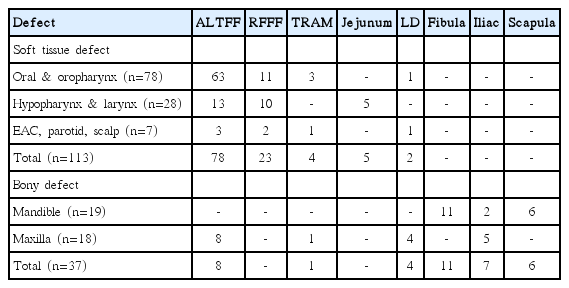
Fig. 1 summarizes all of the free flap cases during the study period. A total of 150 flaps were used in 134 patients. The anterolateral thigh free flap (ALTFF) was most commonly used, being performed in 87 cases and accounting for 69.0% of the soft tissue reconstructive surgeries. The second most common flap was the radial forearm free flap (RFFF), which was performed in 23 cases (18.3%). For the reconstruction of bony defects, the fibular free flap was chosen most frequently, and was used in 44.0% of the cases.
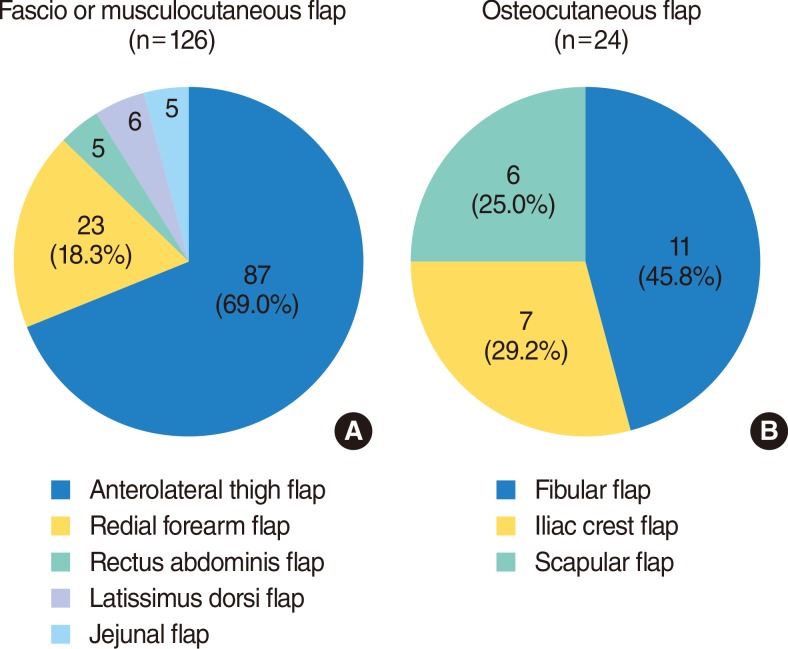
Flaps selected in soft tissue or bony tissue defect reconstruction. (A) The anterolateral thigh flap was most commonly used among various fascio or musclocutaneous flap. (B) The fibular flap was chosen most frequently for the reconstruction of bony defect.
A summary of the defect location and the types of flaps used to reconstruct the defects is provided in Table 1. The majority of the soft tissue defects were located in the oral and oropharyngeal region (n=78, 69.0%). For oral and oropharyngeal defects, the ALTFF was predominantly used and accounted for 80.8% of cases. In other sites, the ALTFF and RFFF were used with similar consistency (45.7% for ALTFF vs. 34.3% for RFFF). All bony tissue defects in the mandible were reconstructed with the osteocutaneous free flap, but only 5 out of 18 cases were reconstructed by iliac osteocutaneous or osteomuscular free flaps in the maxilla.
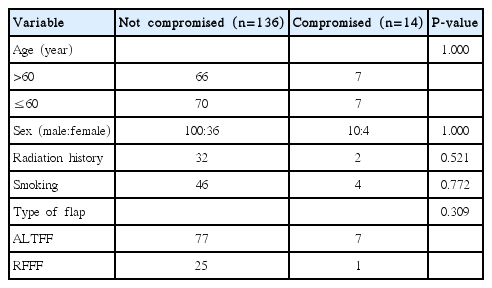
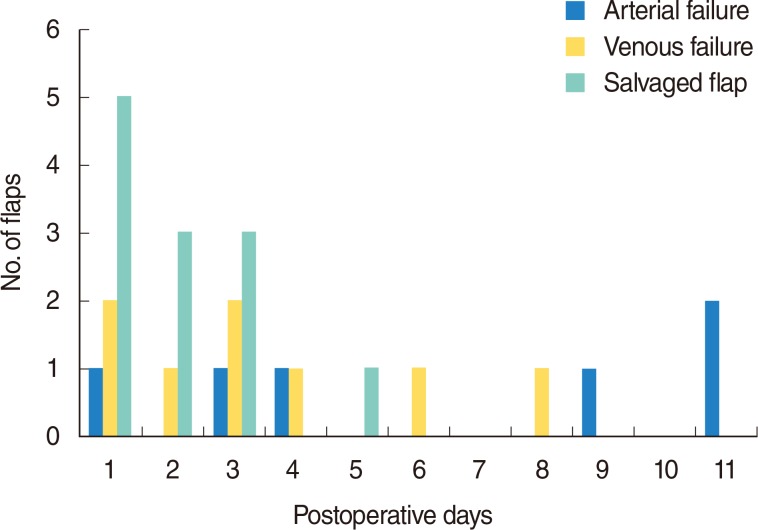
Of 150 flap cases, 14 cases (9.3%) of flap failure occurred and the overall success rate of free flap reconstruction was 90.7%. Table 2 shows the demographic data comparing for risk of flap failure. There was no significant difference between patients with compromised flap and not compromised flap in age, sex, previous radiation history and smoking. In addition, type of flaps did not affect to flap failure. Among the cases of failure, 6 cases were caused by arterial insufficiency and 8 cases involved venous failure. Arterial failure occurred up to 11 days postoperatively, while venous failure occurred within 8 days postoperatively. A total of 19 salvage operations (12.7%) were carried out, and 12 flaps (63.2%) could be salvaged successfully. Salvage due to suspicion of arterial insufficiency was performed in 3 cases. In 2 of these 3 cases, intact arterial pulsation in the pedicle was confirmed and decompression of the tissues surrounding the pedicle was performed; these flaps were found to be stable postoperatively. However, salvage was impossible in the remaining case; therefore, immediate RFFF reconstruction was performed instead of salvage operation. The overall salvage rate for arterial insufficiency was 66.6%.
A salvage operation for venous failure was performed in 16 cases, and 10 cases were successfully salvaged (62.5%). One case showed a twisted pedicle, which was successfully treated by rearrangement of the pedicle. In another case, clinical suspicion of venous congestion led to a salvage reoperation being performed. However, the vessels appeared normal when examined during the operation, so venous anastomosis was performed only for safety. The other 8 cases were salvaged with venous reanastomosis after mechanical thrombectomy.
Most cases of flap compromise occurred in the first 3 postoperative days (17 out of 26 flaps, 65.4%) and 11 of the 12 successful salvage operations were performed during the first 3 days. Although the failed flaps which were managed by the creation of another flap on postoperative days 8, 9, and 11 were detected earlier, the revision operations were postponed due to the poor general condition of these patients. In the case of arterial insufficiency, in particular, it takes time for flap necrosis to become evident, and therefore, the necessary revision surgery is often delayed (Fig. 2).
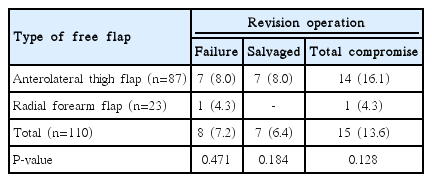
The ALTFF and RFFF, which were the most commonly used flaps, showed a failure rate of 8.0% and 4.3% and a compromise rate of 16.1% and 4.3%, respectively. The ALTFF showed a higher risk of flap failure or compromise than the RFFF, but this difference was not statistically significant (Table 3).
Differences in flap failure and salvage rate according to the primary defect site were explored. The most common site for defects was the oral cavity and the oropharynx, where 102 flaps were used, with a failure rate of 8.8% and a salvage rate of 11.8%. The hypopharynx and larynx (n=28) and the maxilla, hard palate, and nose (n=20) showed a failure rate of 3.5% and 20.0%, respectively. Although there were no statistically significant differences, the maxilla, hard palate, and nose area showed the highest failure rate, while the larynx and hypopharynx had the lowest failure rate. All the successful salvage operations were performed in the oral and oropharyngeal area and there was a difference in the salvage operation rate according to the site of the soft tissue defect (P=0.046). When the total compromise rate was considered, the region of the hypopharynx and larynx showed a lower risk of compromise compared to the oral or maxillary areas (P=0.103) (Table 4).
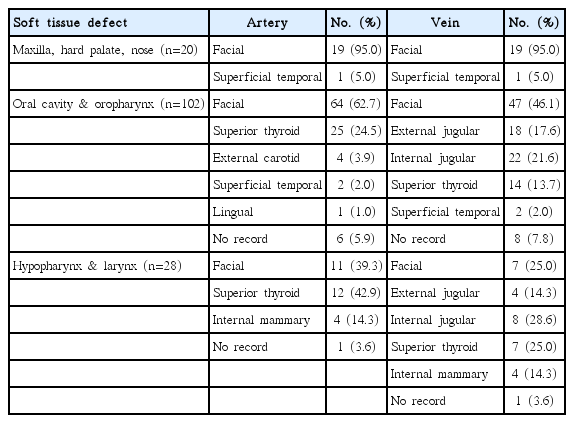
For reconstruction of the maxilla, hard palate, and nose, the facial artery and facial vein were used as the recipient vessels in 95% of cases. For oral and oropharyngeal defects, the facial artery was used in 62.4% of cases and the facial vein was used in 45.5% of cases. Meanwhile, dependency on facial vessels was only 39.3% for the artery and 25% for the vein in the hypopharyngeal and laryngeal area. Dependence on the facial artery and vein was statistically different between sites of the primary defect. (P<0.001 for artery and vein) (Table 5).
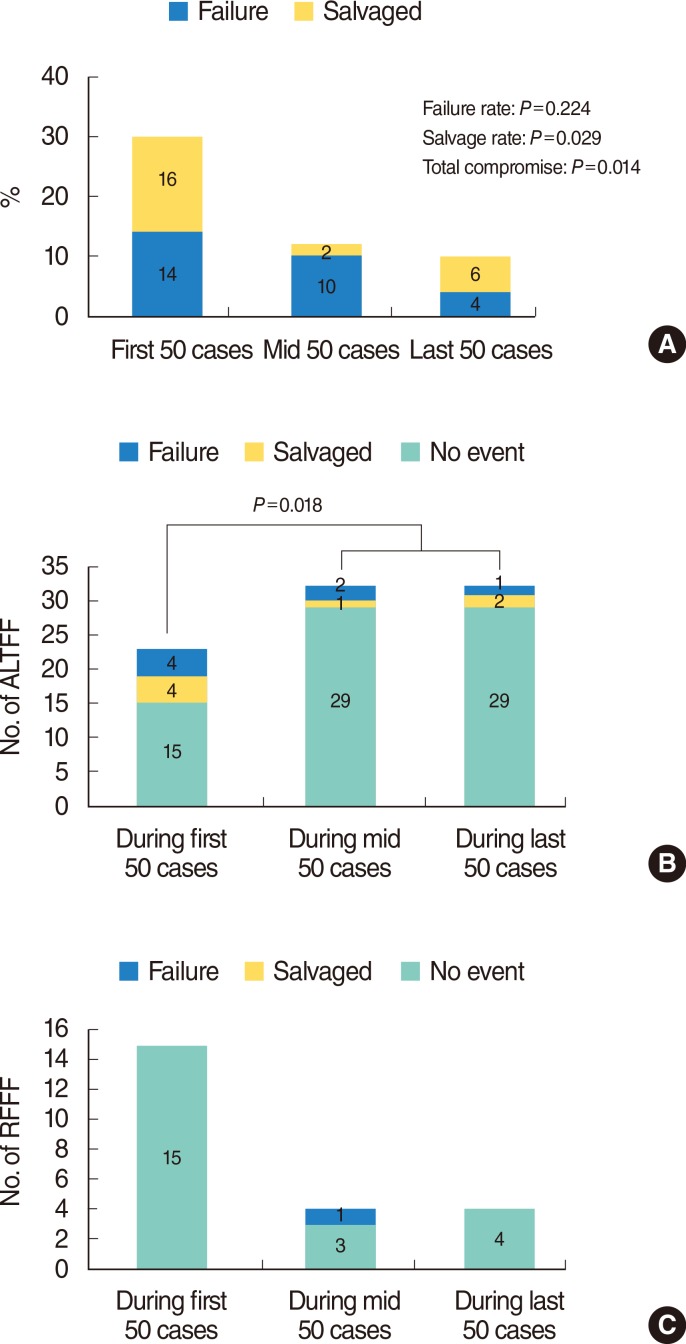
Fig. 3A shows the learning curve for microvascular surgery. During the first 50 cases of free flap reconstruction, a high rate of failure and salvage was experienced (a 30% compromised flap rate and a 14% failure rate). After another 50 cases the compromise rate decreased to 12%, and after 100 further cases, the failure rate was as low as 4%. Although the failure rate was not significantly different between these periods (P=0.224), the compromise rate and the salvage rate were significantly higher in the first 50 cases (P=0.014 and P=0.029, respectively). The results for the ALTFF also followed this learning curve (Fig. 3B). Among the first 50 flaps, 23 ALTFFs were performed. Four cases (17.4%) of flap failure and 4 cases (17.4%) of flap salvage were experienced. In addition, the rate of flap compromise was significantly higher during the first 50 cases (P=0.018). In contrast, the RFFF was performed during the first 50 flaps mostly without flap failure or salvage, and there was only 1 failure during the second 50 flaps. This failure was due to thrombosis of the entire internal jugular vein, and was unrelated to pedicle problems. Unlike the ALTFF, the use of the RFFF was not influenced by experience (Fig. 3C).
DISCUSSION
In this series, the ALTFF was the most commonly used flap among various donor sites. Although the RFFF is very safe and has a suitable appearance for reconstruction, it can cause sensory deficit in 56% of cases and cold intolerance in 39% of cases [5]. The well-known advantages of the ALTFF include the following points: (1) elevation is easy because there are several perforators, (2) the diameter of the vascular pedicle is approximately 2 mm, (3) the flap is potentially sensate because the lateral femoral cutaneous nerve can be used, (4) the skin territory of the ALTFF is very long and wide (about 25 cm long and 18 cm wide), (5) the donor site is far from the head and neck region, and (6) the donor site is hidden and therefore more acceptable to patients [6,7]. For these reasons, the ALTFF is a versatile soft-tissue flap in which the thickness and volume can be adjusted to accommodate the extent of the defect, and is preferred for the reconstruction of defects in the head and neck region, especially in Asia.
The selection of the flap donor site was dependent on the location of the defect. The ALTFF was more frequently used for oral and oropharyngeal defects. For hypopharyngeal and laryngeal defects, the jejunal flap was selected for reconstruction of the cervical esophagus after total laryngopharyngectomy and the RFFF was selected after wide vertical hemilaryngectomy for hypopharyngeal carcinoma [8].
The majority of flap failures occur within the first 72 hours. In a series of 990 patients, Kroll et al. [9] reported that 50 cases (5.1%) developed pedicle thrombosis. Venous thrombosis was more than twice as common as arterial thrombosis and tended to develop later. Hidalgo et al. [10] identified venous problems (35%) as the most common etiology of flap failure followed by arterial problems (28%), hematoma (26%), and recipient vessel problems (11%). Technical errors with flap design and elevation, vessel suturing, tissue handling, and/or geometry of the pedicle may result in thrombosis. Extrinsic compression of the vascular pedicle by tight wound closure, tapes around the neck, or wound hematoma may also compromise the flap by obstruction of the venous outflow [11]. Salvage rates are higher when venous thrombosis is identified as the cause of flap failure. In a review by Nakatsuka et al. [3], arterial thrombectomy was successful in only 15% of cases compared with a 60% salvage rate after venous thrombectomy. This may be related to the fact that venous compromise is easier to detect via traditional methods of monitoring [12]. In our series, problems with the pedicle could be fixed and the flap salvaged in 63.2% of cases. Although the salvage rate of cases involving arterial or venous failure was similar in our series (66.7% and 62.5%, respectively), the two salvage cases involving arterial insufficiency showed no problems with the pedicle itself. Therefore, successful salvage of a compromised pedicle was possible only in the cases of venous failure. In most cases, successful salvage took place within 3 days postoperatively. Careful attention should be paid to the circulation status of the flap during this period and surgeons should be ready to perform revision surgery when vascular compromise is suspected.
The recipient site and choice of recipient vessel may also be factors contributing to the development of flap failure [1,3,13,14], with subsequent reconstruction required for unsalvageable cases. In our experience, dependency on the facial artery and vein was most notable in maxillary, hard palate, and nasal defects, and was the least common in hypopharyngeal and laryngeal defects. This indicates that there is a wider choice of vessels available in the reconstruction of the hypopharynx or larynx. However, for reconstruction in maxillary or hard palate defects, the facial artery and vein are the only option in most cases, in the absence of vein grafts, in most cases. This finding explains the failure and salvage rates according to defect location. As there were no substitutes for the recipient vessels, maxillary and hard palate defects had a high risk of failure. In contrast, in oral and oropharyngeal defects, the facial artery and vein were mainly used but other vessels could also be utilized, and 57% of the compromised flaps were successfully salvaged. In the larynx and hypopharynx, we were also able to use suitable vessels that were a short distance from the defect, and we experienced only one failure without compromise.
When compared to the success rates of up to 99% that were reported in recent studies [15,16], an overall success rate of 90.7% may not appear satisfactory. However, not all surgeons can be expected to be experts from their first case, and as the current analysis includes data from the first case of free flap reconstruction conducted by a single surgeon onwards, the importance of a learning curve for stable microvascular surgery becomes apparent. In addition to surgeon's technique, some confounding factors like sex, age, smoking history, radiation history, and past medical history such as diabetes or vascular disease can affect the flap failure rate. However, in our study, there was no correlation between flap failure and some confounding factors like sex, age, smoking, and previous radiation history. We cannot check all of possible confounding factor such as diabetes or vascular disease, and it is our limitation because of retrospective study. In our series, the salvage rate was decreased to 10% after 100 cases and the failure rate was decreased to 4% with experience. Therefore, for the stabilization of microvascular technique, at least 50 cases may be required.
Since other flaps were not as frequently used, the ALTFF and RFFF fasciocutaneous flaps can be compared. Although the difference was not significant statistically, the ALTFF had higher failure and compromise rates than the RFFF. The variability in the anatomy of the pedicle and the requirement for more technical skill when raising the ALTFF may have contributed to this difference. The importance of adequate salvage surgery should also be highlighted. Another interesting finding was that ALTFFs performed during the first 50 cases showed a significantly higher risk of compromise and followed the general learning curve, while the RFFF did not show compromise or failure even in the early period of practice. This result indicates the safety of the RFFF. The difference may have been due to difficulties in raising the ALTFF and variation in the anatomy and vessel diameter of the ALTFF. Therefore, for the inexperienced microvascular surgeon, selection of the RFFF may be a safer method of reconstruction.
There are 3 main factors contributing to the success of free flap reconstruction. The first is the quality of the surgical procedure. Successful performance of this surgery requires a learning curve, and additionally, caution during arterial anastomosis with a last check of the artery pulse 30 minutes after reperfusion is important to avoid arterial insufficiency, which is difficult to salvage. The preparation of adequate recipient vessels is also important; however, the selection of vessels can be limited by the defect site, and therefore, the checking of potential recipient vessels for intactness should be performed preoperatively. Finally, careful monitoring of the flap in order to detect compromise as soon as possible, with reoperation when flap compromise is suspected, is also important. Using this approach we were able to salvage 63.2% of the flaps which were in danger of failure.
In conclusion, the free flap technique is safe but involves a learning period for the surgeon and careful postoperative monitoring of the patient. The highest success rates were seen in laryngeal and hypopharyngeal reconstruction; this was due to wider choice of substitutes of the recipient vessels than in other sites. Early intervention is important for the salvage of free flaps and 63.2% of the compromised flaps were salvaged with immediate exploration. In addition, achieving consistent success using microvascular techniques requires a learning curve.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.