Comparison of Short- and Long-term Hearing Outcomes of Successful Inlay Cartilage Tympanoplasty Between Small and Large Eardrum Perforations
Article information
Abstract
Objectives
To compare the short- and long-term hearing outcomes after successful inlay cartilage tympanoplasty between patients with small (≤25%) and large (≥50%) eardrums perforations.
Methods
This is a retrospective case series study conducted in a tertiary referral center. Twenty-five patients who underwent 27 procedures were enrolled. Their mean age was 60.26 years (range, 42 to 76 years). The mean follow-up time was 18.86 months (range, 12.30 to 35.83 months). The preoperative, initial postoperative, and long-term hearing results in patients with total repair of the eardrum were analyzed.
Results
In the small size group, the average (±standard deviation) air-bone gap (ABG) closure was 1.08±7.53 dB in the short-term and 2.33±11.56 dB in the long-term hearing examinations. There was no difference between short- and long-term ABG closure (P=0.689). In the large size group, the average ABG closure was 9.77±9.40 dB in the short-term and 16.25±6.01 dB in the long-term hearing examinations. There was a significant difference between short- and long-term ABG closure (P=0.029).
Conclusion
Patients with large perforations have continuous hearing improvement and ABG closure for more than one year. In contrast, the short- and long-term postoperative ABGs are almost the same in patients with small perforations. More long-term postoperative follow-up of hearing results is necessary for large perforations.
INTRODUCTION
Tympanoplasty is the most common procedure for eardrum perforation in otorhinolaryngology departments. Inlay cartilage tympanoplasty (ICT) technique was first introduced by Eavey [1] for closure of small-to-medium sized central perforations in 1998. ICT has also evolved from small-to-medium sized tympanic perforations [23456] to more extensive ear surgery [78910]. It has several practical advantages, such as local anesthesia, small incision, transcanal route, and short surgical time, when comparing the traditional underlay tympanoplasty [11]. In a previous study, the take rate and audiometric results of ICT procedures are similar to traditional underlay tympanoplasty [11]. Younger patients and those with larger perforations >50% are more likely to benefit from this procedure [9].
Another study has reported on the short- and long-term hearing outcomes of successful ICT that compared between patients older and younger than 60 years old. Improvements in hearing continued for more than one year after surgery, especially in patients younger than 60 years old. The present study compared the short- and long-term hearing outcomes after ICT between patients with small- and large-sized eardrum perforations.
MATERIALS AND METHODS
After approval by the Institutional Review Board of Chang Gung Memorial Hospital (IRB No. 103-2677B), a retrospective cohort was conducted to identify the hearing patterns of patients who received ICT. All procedures were conducted by one senior surgeon (WHW) of the Department of Otolaryngology at Chiayi Chang Gang Memorial Hospital between March 2006 and March 2008.
The inclusion criteria were (1) stable eardrum perforation for more than one year; (2) dry ear without otorrhea at the time of surgery; and (3) nonmarginal perforation and sufficient width of the ear canal; (4) patients who were followed-up for more than one year. Those without sufficient follow-up data for one year after surgery, without preoperative hearing tests, without postoperative hearing tests at least twice, and failed graft or any wound infections were excluded. The characteristics of the patients and diseases were collected. Successful surgery was defined as complete tympanic membrane healing without retraction or lateralization on the last visit. The preoperative, initial postoperative, and long-term hearing levels in patients with total repair of the eardrum were analyzed. Four patients were excluded due to failed graft.
Surgical techniques
The modified ICT procedure described by Lubianca-Neto [3] was performed in this study. Topical anesthesia with lidocaine and epinephrine 1:100,000 was injected subcutaneously into the tragus and external ear canal. The tragal cartilage with the perichondrium preserved on one surface was harvested first. The perichondrium was preserved on only one side (the outer side) based on clinical experience, thereby making it easier to approach the perforation site. Denuding around the perforation was done under a microscope and a butterfly graft was then created with a mini-blade. The graft was grasped by the alligator forceps and inserted to the perforation via transcanal method.
Simple myringoplasty without any ossicular reconstruction was performed for all cases. No external ear canal, mastoid packing, or any graft stability method was needed. Postoperative prophylactic antibiotics were prescribed for three days and local wound cleaning was scheduled once a week until good healing. There was no infection in any of the patients.
Otoscope image recording and hearing tests
All of the patients were assessed by clinical history, general physical and otorhinolaryngologic examinations, audiometry, imaging studies, and preoperative tests. The eardrum with an otoscope in every pre- and postoperative clinical follow-up was observed (Fig. 1). The mean values of tonal audiometry were calculated using values from 0.5, 1, 2, and 4 kHz in a study of the air and bone conduction curves.
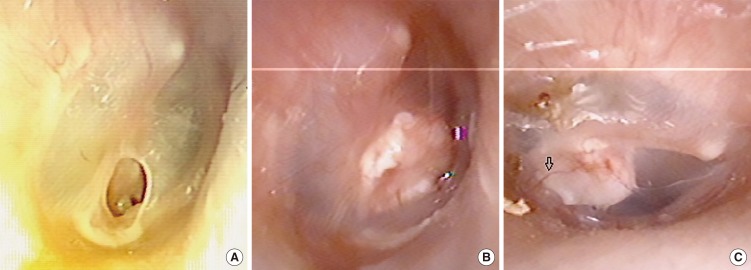
Otoscope image of eardrum preoperatively (A), one month (B), and three months (C) postoperatively. Arrow indicates neovessel ingrowth on the outer surface of cartilage.
Pure tone audiometry (PTA) with air and bone conduction was done for an average of six and 18 months after surgery. Short-term hearing examination was defined as the first hearing examination after surgery. Because older patients suffered from hearing loss with age during the long-term follow-up period, the hearing threshold gain was adjusted in order to exclude the aging effect (presbycusis) by subtracting the degree of deterioration of the normal contralateral ear from the hearing threshold value of the operated ear.
The hearing levels of each frequency were recorded both in air conduction (0.25, 0.5, 1, 2, 4, and 8 kHz) and bone conduction (0.5, 1, 2, and 4 kHz). The mean hearing levels were defined as the average of hearing levels at frequencies of 0.5, 1, 2, and 4 kHz. The air-bone gap (ABG) was defined as the average of the air-bone conduction gap at 0.5, 1, 2, and 4 kHz.
Statistical analyses
Audiometric data were expressed as mean (±standard deviation [SD]) hearing level, hearing gain, ABG, and ABG closure, and were compared using paired t-test. Categorical variables were compared using the chi-square test or Fisher exact test. Data were statistically analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Significance was set at P<0.05.
RESULTS
Table 1 summarized the hearing outcomes of all patients. Twenty-seven ears of 25 patients (10 males and 15 females) were enrolled. Two patients received bilateral surgery at the same time. Ten were left ear and 17 were right ear. The mean patient age was 60.26 years (range, 42 to 76 years). Sixteen ears had small eardrums perforation size (≤25%) and 11 ears had large perforations (≥50%). The mean follow-up time was 18.86 months (range, 12.30 to 35.83 months).
Pure tone hearing thresholds change
The average short-term PTA was 6.09 months (range, 5.10 to 7.30 months) after surgery. Long-term hearing examinations were performed on the last clinical visit, and all were done more than one year after surgery (mean, 18.86 months; range, 12.30 to 35.83 months).
Among the patients with small perforations, the mean preoperative, postoperative short-term, and postoperative long-term hearing thresholds were 47.27±14.53, 46.56±16.11, and 49.06±19.14 dB, respectively. The average hearing gain was 0.7±7.19 dB in the short-term and -1.8±13.19 dB in the long-term hearing examinations.
Among the patients with large perforations, the mean preoperative, postoperative short-term, and postoperative long-term hearing thresholds were 59.66±15.55, 50.57±20.60, and 44.89±21.95 dB, respectively. The average hearing gain was 9.09±10.13 dB in the short-term and 14.77±9.35 dB in the long-term hearing examinations.
Comparing the two groups (Table 1), the large perforation group had poor preoperative hearing thresholds but the difference between the two groups was not statistically significant (P=0.052). The large perforation group also had significantly better short- and long-term hearing gain (P<0.05) after surgery. Thus, there was no difference in postoperative short- and long-term hearing thresholds between the two groups (P>0.05).
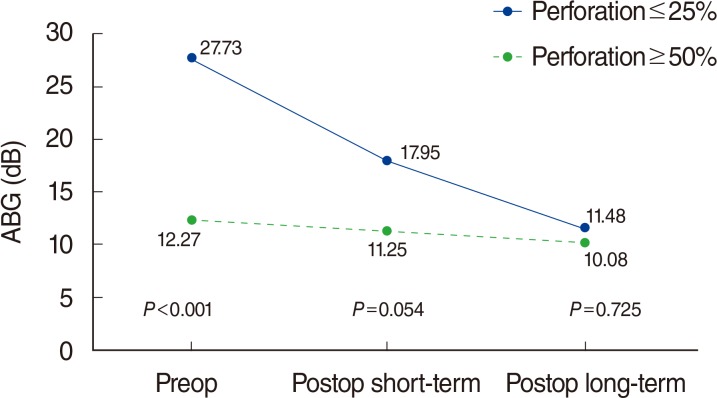
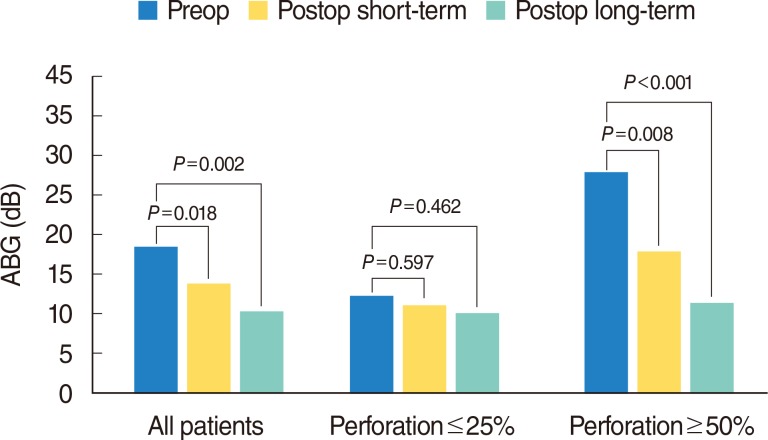
ABG closure change
Among the patients with small perforations, the mean preoperative, postoperative short-term, and postoperative long-term ABGs were 12.27±6.65, 11.25±7.07, and 10.08±10.60 dB, respectively (Fig. 2). The average ABG closure was 1.08±7.53 dB in the short-term and 2.33±11.56 dB in the long-term hearing examinations. There was no difference between the short-term and long-term ABG closure (P=0.689) after surgery in this group (Fig. 3).
The mean preoperative, postoperative short-term, and postoperative long-term air-bone gap. Preop, preoperative; Postop, postoperative; ABG, air-bone gap.

The mean postoperative (postop) short- and long-term air-bone gap (ABG) closure after inlay cartilage tympanoplasty.
Among the patients with large perforations, the mean preoperative, postoperative short-term, and postoperative long-term ABGs were 27.73±8.29, 17.95±9.51, and 11.48±21.95 dB, respectively (Fig. 2). The average ABG closure was 9.77±9.40 dB in the short-term and 16.25±6.01 dB in the long-term hearing examinations. There was a significant difference between the short-term and long-term ABG closure after surgery in the large size group (P=0.029) (Fig. 3).
Comparing the two groups (Table 1), the large perforation group had more ABG than the patients with small perforation preoperatively (P<0.001). However, there was no difference in postoperative short-term (P=0.054) and long-term ABGs (P=0.725) (Fig. 4). The difference in ABGs between the two groups decreased over time because hearing improvement and ABG closure continued in the large perforation group. However, the short-term and long-term postoperative ABGs were almost the same in the small perforation group (Figs. 2, 4).
DISCUSSION
Ghanem et al. [7] reported a series of patients aged from 2 to 20 years who received ICT for large perforations with mean follow-up duration of 27.6 months. In their study, the mean preoperative to postoperative four-tone ABG improved from 23 to 21 dB, and the number of patients with 0 to 10 dB hearing results increased from 16 ears preoperatively to 32 ears postoperatively. Yu and Yoon [12] studied 17 patients (range, 9 to 64 years) with bilateral perforated chronic otitis media. They underwent conventional tympanoplasty/mastoidectomy on the first ear and same-day ICT on the contralateral ear with small-to-medium perforations. The median follow-up duration of was 13.0 months and the mean ABG improved from 15.8 to 8.4 dB. Twelve patients had an average ABG between 0 and 10 dB, three between 11 and 20 dB, and two between 21 and 30 dB. The time of the postoperative audiometry performed were not mentioned.
Onal et al. [13] studied the long-term (the mean±SD follow-up period was 24.9±13.4 months in the fascia group and 20.9±9.3 months in the cartilage group) functional results of temporalis fascia versus ICT in patients with bilateral chronic otitis media. Postoperatively, the mean±SD air conduction threshold was 28.54±14.20 dB for the fascia group and 22.97±8.37 dB for the cartilage group, while the mean±SD bone conduction threshold was 11.71±8.50 dB for the fascia group and 7.15±5.56 dB for the cartilage group. However, they did not report any short-term data to know when functional results were achieved.
The time of postoperative audiometry was performed 3-6 months after surgery or was not mentioned in most of the literature [1234567891011]. In the current study, the average time for short-term audiometry was 6.09 months (range, 5.10 to 7.30 months) after surgery. The long-term hearing examinations were performed more than one year after surgery (mean, 18.86 months; range, 12.30 to 35.83 months). This made the study possible to compare dynamic hearing change after ICT.
In the current study, the large perforation group had continuous hearing improvement and ABG closure for more than one year. The long-term ABG closure was significantly better than that in short-term after surgery (P<0.05) (Fig. 2). However, the short- and long-term postoperative ABGs were almost the same in the small perforation group (Figs. 2, 4). The large perforation group had more ABG than the small perforation group, preoperatively (P<0.001). The difference in ABGs between the two groups decreased over time after surgery because hearing improvement and ABG closure continued in the large perforation group (Fig. 4).
Although it is generally accepted that hearing is not the only purpose of tympanoplasty, improved hearing undoubtedly improves the quality of life and thus plays a major role in the patient's expectations. Based on the results, when performing ICT on patients with large eardrum perforation (≥50%), recovery of hearing may take longer time than that in patients with small perforation, or even longer time than that in patients who undergo traditional underlay tympanoplasty.
The compliance and vibration of both eardrum and ossicle chain attribute to the ABG closure. We hypothesized that a larger graft is more likely to be in direct contact with the malleus, causing the "fourth ossicle" effect as a possible reason why individuals with larger perforations had better ABG closure in our previous study [9]. The connection between cartilage graft and tympanic membrane and malleus should be important for acoustic transfer. Furthermore, large eardrum perforation may require longer time for healing and tissue remodeling between the cartilage graft and original tympanic membrane, and even the malleus. Implanted cartilage remodeling with time was also observed after surgery (Fig. 1). These may be the reason why ABG closure continued to improve in the patient with large perforation during the follow-up period.
To date, this is the first study to focus on comparing short- and long-term hearing outcomes between the patients with small (≤25%) and large (≥50%) eardrum perforation after ICT in a retrospective adult series. However, this study has the limitation of being relatively small number of cases because of the retrospective study design. More studies with high number of cases or prospective studies are needed to prove this assertion.
In conclusion, patients with large perforations have continuous hearing improvement and ABG closure for more than one year. In contrast, the short- and long-term postoperative ABGs are almost the same in patients with small perforations. More long-term postoperative follow-up of hearing results is necessary for large perforations.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.