Congenital Stapes Anomalies with Normal Eardrum
Article information
Abstract
Objectives
A non-progressive and conductive hearing loss with normal eardrum, but no history of trauma and infection, is highly suggestive of a congenital ossicular malformation. Among ossicular anomalies, stapes anomaly is the most common. The purpose of this study is to describe patterns of stapes anomaly and to analyze its surgical outcome with special reference to its patterns.
Methods
We conducted a retrospective case review. The subjects comprised 66 patients (76 ears) who were decisively confirmed by the exploratory tympanotomy as congenital stapes anomalies without any anomalies of the tympanic membrane and external auditory canal. The preoperative and postoperative audiological findings, temporal bone computed tomography scan, and operative findings were analyzed.
Results
There were 16 anomalous patterns of stapes among which footplate fixation was the most common anomaly. These 16 patterns were classified into 4 types according to the status of stapes footplate. Successful hearing gain was achieved in 51 out of 76 ears (67.1%) after surgical treatment.
Conclusion
Footplate fixation was usually bilateral, whereas stapes anomalies associated with other ossicular anomaly were usually unilateral. The success of the surgical treatment of stapes anomaly might depend on its developmental status of the footplate. Stapes anomalies were detected without any fixed patterns, therefore, it is quite possible to detect a large variety of patterns in future.
INTRODUCTION
Congenital anomalies of ossicle in the middle ear is rare, however, may present in a variety of ways. Ossicular deformities may occur in a normal tympanic membrane and external auditory canal because the tympanic membrane and external auditory canal do not derive from the same embryological origins as the ossicles. Nevertheless, they are clinically important because hearing loss can be corrected by an appropriate procedure. A non-progressive and conductive hearing loss with a normal eardrum, but no history of trauma or infection, is highly suggestive of a congenital ossicular anomaly, and stapes anomaly is the most common among the ossicular anomalies. Until now, there are many reports published about histopathology and surgical result of congenital anomalies of the stapes with no malformations of the external ear (1-7), and it has commonly been believed that the stapes footplate fixation at one or multiple points is perhaps the most common isolated middle ear anomaly (8, 9). The purpose of this study is to describe patterns of stapes anomalies encountered in patients who have a normal eardrum, and to analyze its surgical results with special reference to the patterns of stapes anomalies.
MATERIALS AND METHODS
This retrospective review was performed at the Department of Otolaryngology, Ajou University Hospital from 1994 to 2006. The subjects comprised 66 patients (76 ears), and the exploratory tympanotomy confirmed all of them as congenital stapes anomalies without any anomalies of the tympanic membrane and external auditory canal. Patients with a previous history of head injury or of a progressive hearing loss were excluded. There was no difference in distribution of gender, and the average age at diagnosis was 24.3 yr (8-58 yr). The average air conduction threshold level at 0.5, 1, 2, and 3 kHz before surgery was 50.9±7.2 dB, and the preoperative air-bone gap (ABG) was 34.5±7.9 dB. Malformations of the ossicles were described on the basis of operative findings and preoperative temporal bone computed tomography findings. Described patterns of anomalous stapes were also classified into 4 types according to the status of the stapes footplate. Stapes fixation was confirmed by operative findings including manual palpation and RW reflex. Based on operative finding, audiometric, and computed tomography (CT) scan criteria, stapes anomaly was considered to be unilateral or bilateral. Surgical result was analyzed with special reference to classified anomalies. Surgical procedure consisted of stapedotomy (53 cases) or stapedectomy (3 cases) in cases with stapes fixation, ossiculoplasty with total ossicular replacement prosthesis (TORP) in cases with mobile footplate, and no additional procedure in cases without stapes footplate and oval window. The postoperative audiometric follow-up was performed at least 3 months after surgery. Hearing outcomes were reported in accordance with the 1995 guidelines of the Committee on Hearing and Equilibrium for both preoperative and postoperative results. Postoperative ABG (postoperative air conduction - preoperative bone conduction) to within 20 dB was considered as a successful outcome (10). Fisher's exact test was used for statistical analyses of the data using SPSS ver. 12.0 (Chicago, IL, USA). Cases in which the P-value was <0.05 were considered statistically significant.
RESULTS
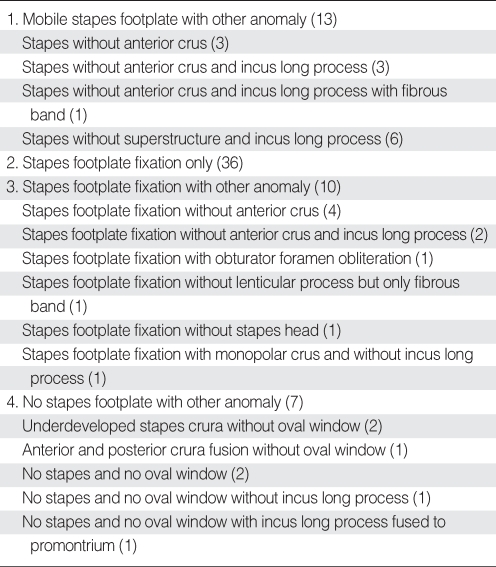
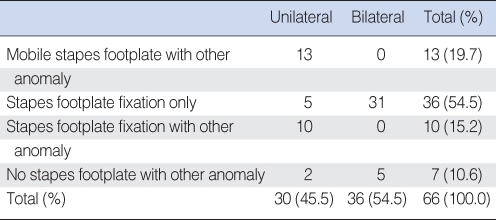
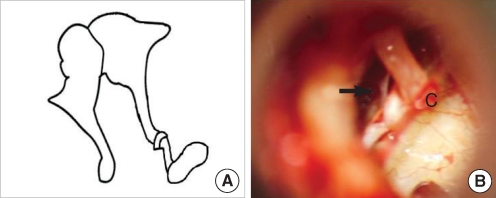
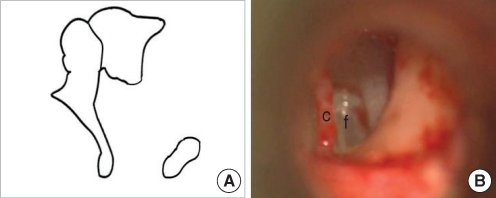
Anomalies of 66 cases could be categorized into the following 16 patterns: stapes without anterior crus (3 cases, Fig. 1); stapes without anterior crus and incus long process (3 cases, Fig. 2); stapes without anterior crus and incus long process with fibrous band (1 case, Fig. 3); stapes without superstructure and incus long process (6 cases, Fig. 4); stapes footplate fixation (36 cases, Fig. 5); stapes footplate fixation without anterior crus (4 cases, Fig. 6); stapes footplate fixation without anterior crus and incus long process (2 cases, Fig. 7); stapes footplate fixation with obturator foramen obliteration (1 case, Fig. 8); stapes footplate fixation without lenticular process but only fibrous band (1 case, Fig. 9); stapes footplate fixation without stapes head (1 case, Fig. 10); stapes footplate fixation with monopolar crus and without incus long process (1 case, Fig. 11); underdeveloped stapes crura without oval window (2 cases, Fig. 12); anterior and posterior crura fusion without oval window (1 case, Fig. 13); no stapes and no oval window (2 cases, Fig. 14); no stapes and no oval window without incus long process (1 case, Fig. 15); and no stapes and no oval window with incus long process fused to promontrium (1 case, Fig. 16). Among the above described 16 patterns of congenital stapes anomalies, stapes footplate fixation was the most common. These 16 patterns of congenital stapes anomaly were classified into 4 types according to the status of stapes footplate (Table 1). As for the stapes anomaly, 36 cases (54.5%) were bilateral (Table 2). When anomalies were confined to stapes, they were usually bilateral. In cases with only stapes footplate fixation, 31 out of 36 patients (86.1%) were bilateral. When stapes footplate fixation was combined with other anomaly, 10 out of 10 cases (100.0%) were unilateral (Table 2). Exploratory tympanotomy was performed on 76 ears of 66 patients, and hearing results according to 4 types of the status of the stapes footplate are summarized in Table 3. Mean postoperative air conduction was 29.7±15.3 dB and postoperative ABG (postoperative air conduction-preoperative bone conduction) was 13.3±13.1 dB. There was one case of postoperative sensorineural hearing loss defined as more than 15 dB loss of bone conduction after surgery. Patients with mobile stapes or only stapes footplate fixation had significantly better hearing result than patients with stapes fixation associated with other ossicular anomaly or no stapes footplate (Fig. 17). Successful hearing gain was achieved in 51 out of 76 ears (67.1%) after surgical treatment.
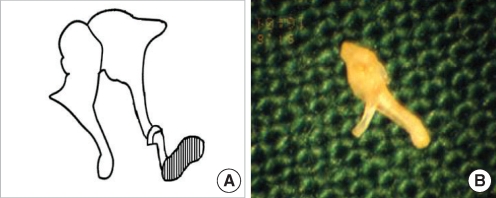
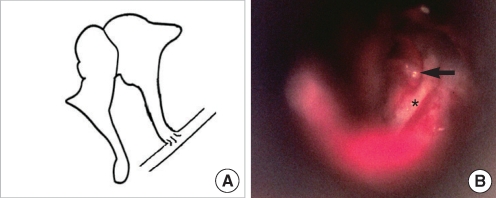
Stapes without anterior crus. (A) Schematic presentation. (B) Operative finding shows no anterior crus of the stapes (arrow).
c: chorda tympani.

Stapes without anterior crus and incus long process. (A) Schematic presentation. (B) Removed incus shows no long process, and removed stapes shows no anterior crus.

Stapes without anterior crus and incus long process with fibrous band. (A) Schematic presentation. (B) Operative finding shows a fibrous band (arrow) instead of the incus long process and the stapes lacking anterior crus (asterisk).
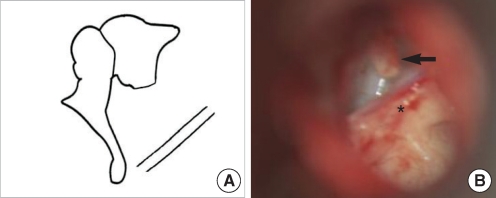
Stapes without superstructure and incus long process. (A) Schematic presentation. (B) Operative finding shows no incus long process and no stapes superstructure.
c: chorda tympani; f: footplate.

Stapes footplate fixation. (A) Schematic presentation. (B) Operative finding shows half of the stapes footplate remaining (arrow) because of partial fixation of its footplate.
Stapes footplate fixation without anterior crus. (A) Schematic presentation. (B) Removed stapes shows an underdeveloped anterior crus.
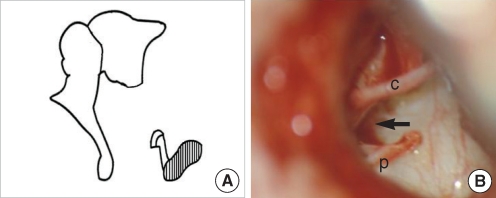
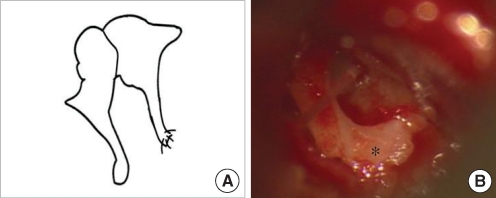
Stapes footplate fixation without anterior crus and incus long process. (A) Schematic presentation. (B) Operative finding shows no incus long process and the stapes lacking anterior crus (arrow) without mobility of its footplate. c: chorda tympani; p: posterior crus.

Stapes footplate fixation with obturator foramen obliteration. (A) Schematic presentation. (B) Removed stapes shows a non-perforated obturator foramen.

Stapes footplate fixation without lenticular process: only fibrous band. (A) Schematic presentation. (B) Operative finding shows a fibrous band (arrow) instead of the lenticular process of the incus.
c: chorda tympani.
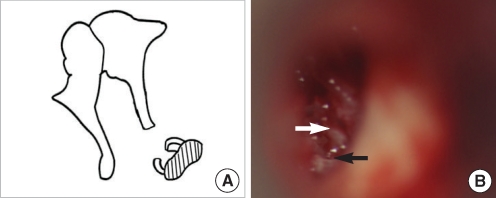
Stapes footplate fixation without stapes head. (A) Schematic presentation. (B) Operative finding shows only anterior (white arrow) and posterior crus (black arrow) without mobility of its footplate.

Stapes footplate fixation with monopolar crus and without incus long process. (A) Schematic presentation. (B) Operative finding shows only one crus in the center of the footplate (arrow) and stapes-pyramidal fixation by a bony bar (asterisk).

Underdeveloped stapes crura without oval window. (A) Schematic presentation. (B) Removed stapes shows underdeveloped crura.
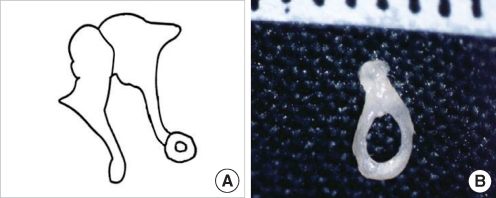
Anterior and posterior crura fusion without oval window. (A) Schematic presentation. (B) Removed stapes shows a crural fusion.
No stapes and no oval window. (A) Schematic presentation. (B) Operative finding shows a long process of the incus (arrow) without the stapes, which is in contact with a downward facial nerve (asterisk) in the mesotympanum.
No stapes and no oval window without incus long process. (A) Schematic presentation. (B) Operative finding shows shortening of the incus long process (arrow) without the stapes and downward displacement of the tympanic portion of the facial nerve with a bony bar (asterisk).
No stapes and no oval window with incus long process fused to promontorium. (A) Schematic presentation. (B) Operative finding shows the long process of the incus fused to promontorium (asterisk) without the stapes and the oval window.
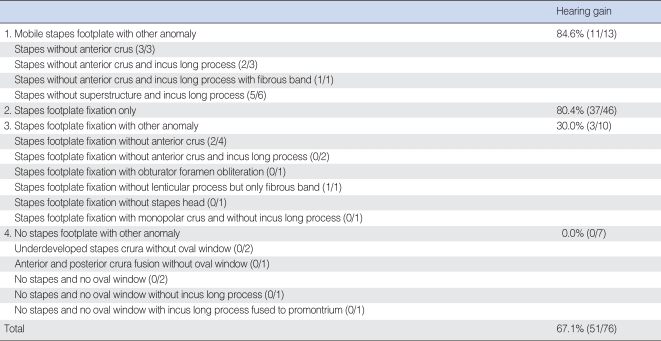
Hearing results of congenital stapes anomaly according to status of stapes footplate after more than 3 months of surgery (76 ears)
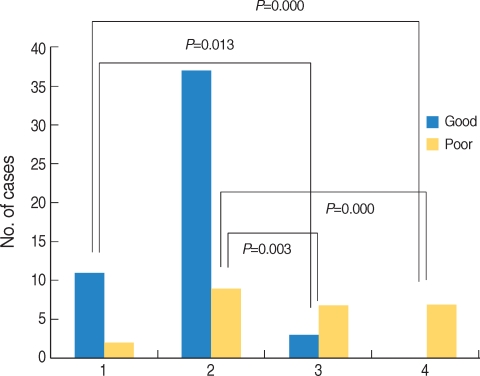
Comparison of postoperative hearing results of congenital stapes anomaly according to status of stapes footplate (76 ears). Patients with mobile stapes or only stapes footplate fixation had significantly better hearing result than patients with stapes fixation associated with other ossicular anomaly or no stapes footplate.
1: Mobile stapes footplate with other anomaly; 2: Stapes footplate fixation only; 3: Stapes footplate fixation with other anomaly; 4: No stapes footplate with other anomaly; Good: postoperative air-bone gap <20 dB; Poor: postoperative air-bone gap ≥20 dB. Postoperative air-bone gap: postoperative air conduction-preoperative bone conduction.
DISCUSSION
The upper ossicular chain is closely related more to the first branchial arch, whereas the lower ossicular chain is related to the second arch. For this reason, it is common to find malformations of the lower half of the ossicular chain in conjunction with marked stapes anomalies. Anatomic variations of the stapes may differ considerably in type and extent (11), and it is very difficult to appreciate why anomalies were involved more in the second arch-originated ossicles, restricted only to the stapes, and not involved in the other ossicles even from the same arch. Although congenital anomalies of the stapes without malformations of the external ear are not common, high resolution CT of the temporal bone and exploratory tympanotomy provide otologic surgeons with a greater chance of revealing them.
The most common congenital isolated ossicular anomalies are stapes fixation and incudostapedial discontinuity (12), and isolated congenital stapes fixation represents 20% to 35% of ossicular malformations (5, 13, 14). It is of a great interest to note that isolated stapes footplate fixation comprised more than 50% in this study. Congenital stapes fixation is the result of a fixation between the peripheral lamina stapedialis and the annular ligament (15), and it is the cause of conductive deafness with a normal tympanic membrane. The differential diagnosis of stapes fixation includes other ossicular malformations, oval or round window atresia, congenital cholesteatoma at early stage or other middle ear tumors, and ossicular trauma (7). Congenital stapes fixation must be distinguished from stapes otosclerosis which is defined by a progressive deafness, even if the surgical procedures are the same. Thus, the nonprogressive deafness is an essential element of the diagnosis, which is easy to establish, when patients are followed regularly with clinical examination and unchanged audiometric thresholds.
In this study, bilateral stapes anomaly was found in 36 out of 66 cases (54.5%), and 31 out of 36 (86.1%) cases of stapes fixation were bilateral in consistence with other studies which range from 68% to 90% (5, 7).
Another interesting finding in this study was that there were no stapes anomalies combined with the malleolar anomalies, and stapes anomalies associated with other ossicular anomalies were unilateral.
Recently, there have been increasing number of reports on the cases with stapes anomalies other than footplate fixation (16-21). However, most of stapes anomalies in these reports were found to be associated with stapes fixation. In our present study, however, 19.7% of all stapes anomaly cases involved mobile stapes footplate.
Earlier studies showed that audiometric results after surgical treatment of middle ear malformation are better for congenital stapes ankylosis, particularly if no other middle ear malformation is associated (5, 17). In this study, patients with mobile stapes or only stapes footplate fixation had significantly better hearing outcomes than patients with stapes fixation associated with other ossicular anomaly or no stapes footplate. Furthermore, Teunissen et al. (5) reported poor surgical outcome in cases associated with stapes superstructure anomaly, in agreement with our result. Therefore, it is quite likely that well developed stapes is important in hearing improvement.
CONCLUSION
In this study, we found that most of the footplate fixation were bilateral, whereas stapes anomalies associated with other ossicular anomaly were unilateral. The success of the surgical treatment of stapes anomaly might depend on developmental status of the footplate. Stapes anomalies were detected with no fixed patterns, therefore, it is expected to detect a large variety of these patterns in future.
Notes
All authors had no conflict of interest on this study.