Association Between Interleukin-6 and Head and Neck Squamous Cell Carcinoma: A Systematic Review
Article information
Abstract
Interleukin-6 (IL-6) is a proinflammatory cytokine which plays an important role in several regulatory mechanisms of cancer. Moreover, experimental and clinical studies have reported that IL-6 targeted therapies might provide significant benefits for cancer treatment. The purpose of this systematic review is to evaluate IL-6 activity in patients with head and neck squamous cell carcinoma (HNSCC). A systematic review of the association between serum, saliva and tumor IL-6 and HNSCC was developed on PubMed/Medline in the publication range from January 1995 to January 2019. Our literature analysis demonstrated that overexpression and elevated serum and/or saliva IL-6 concentrations in patients with HNSCC are related to poor survival and oncological outcomes. Although there is a correlation between IL-6 concentrations and tumorigenicity, it is noteworthy that IL-6 targeted therapies are generally performed in vitro and in experimental studies. Therefore, prospective, randomized clinical trials are required that focus on IL-6 targeted therapies for the treatment of HNSCC.
INTRODUCTION
Head and neck cancer (HNC) is the sixth most common cancer worldwide and accounts for more than 600,000 new cases every year [1,2]. In 1990, the US economic burden of HNC was approximately 1 billion dollars annually [1]. Squamous cell carcinoma, which mainly arises from the mucosa lining the aerodigestive system, is the most common histopathological type of HNC [3]. Despite tremendous advances in the fields of diagnosis and treatment, survival outcomes are still suboptimal with a 5-year survival rate of less than 50% [4]. Hence, diagnostic (benign vs. malignant), predictive and prognostic biomarkers for head and neck squamous cell carcinoma (HNSCC) are urgently required in order to attain satisfactory clinical and oncological outcomes. To date, a variety of biological materials (serum, saliva, tumor specimens, body fluids, etc.) have been tested as tumor biomarkers for HNSCC [5-12]. Disappointingly, an ideal “biomarker” for HNSCC has not emerged for clinical use yet. Nevertheless, the quest for a well-validated, highly sensitive and specific “biomarker” still continues.
Recently, a variety of clinical and experimental studies have determined the key roles of interleukin-6 (IL-6) in several mechanisms of various cancers such as lymphoma, multiple myeloma, prostate, bladder, breast and colorectal cancers [13-17]. IL-6 is a multifunctional and pleiotropic cytokine which is secreted from monocytes, fibrocytes, keratinocytes, endothelial cells, adipocytes, T- and B-lymphocytes, and cancerous cells. It is one of the major regulators of the immune system and orchestrates several biological events such as inflammation, hematopoiesis, acute phase response, cellular proliferation and differentiation, apoptosis and carcinogenesis. IL-6 signals through two different receptors: IL-6 receptor (IL-6R) and gp130. In human, while all cells are able to excrete the gp130 receptor, IL-6R is unique and exclusively excreted by hepatocytes, neutrophils, monocytes/macrophages and lymphocytes. Both of these receptors are located in the cell membrane and plasma. It is noteworthy that activation of the signaling pathway (canonical signaling pathway or trans-signaling pathway) occurs according to the interaction of IL-6 with different receptors. In addition, deactivation of these signaling pathways occurs when these receptors are blocked (Fig. 1A-C).
(A-C) The activation of interleukin-6 (IL-6) signaling pathway. (D) IL-6 signaling pathways activated the Janus tyrosine kinase (JAK-STAT), PI3K signaling pathways and the Ras-MAPK mitogen activated protein kinase pathways which have several effects on inflammatory, autoimmune or malignant diseases.
In the canonical signaling pathway (membrane bound IL-6R [mbIL-6R] (+) and membrane bound gp130 [mbgp130—common signal transducing component of IL-6 receptor] (+) cells), the dimerization of IL-6 with membrane bound IL-6R and membrane bound gp130 results in a high affinity functional receptor complex called IL-6/IL-6R/gp130 (Fig. 1A). The Janus tyrosine kinase (JAK-STAT) and PI3K signaling pathways and the Ras-MAPK mitogen activated protein kinase pathways are activated by this functional complex, and play an essential role in several inflammatory, autoimmune and malignant diseases. In mbIL-6R negative or low secreted cells, after complexing of IL-6 and sIL6R, this complex binds to mbgp130 and the signal pathway will be activated; this is called the “trans-signaling pathway” (Fig. 1B). Due to activation of this pathway, it is possible that the cells which are not responsive to IL-6 under normal conditions are activated by sIL-6R. In fact, 70% of the secreted IL-6 is complexed with sIL-6R and binds directly to mbgp130 protein while the other portion remains in serum temporarily and binds directly to mbIL6R. Finally, the complex of sIL-6R/IL-6 in serum leads to inactivation of IL-6 as a consequence of sGP130 binding (Fig. 1C).
Currently, it is known that IL-6 plays a key role in several “hallmarks” (tumorigenesis, inducing angiogenesis, sustaining proliferative signaling, etc.) of solid cancers via triggering downstream activation of the JAK-STAT and PI3K signaling pathways (Fig. 1D). Thereby, dysregulation of IL-6 signaling promotes cancer cell proliferation and survival intrinsically and supports tumor growth via activating angiogenetic factors extrinsically. Hence, the purpose of this systematic review is to present a comprehensive and contemporary view of the association between IL-6 and different clinical and oncological aspects of HNSCC.
MATERIALS AND METHODS
A systematic literature search was developed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and performed on PubMed/Medline in the publication range from January 1995 to January 2019. The search terms were as follows: (interleukin 6) AND (head neck squamous cancer OR head neck squamous carcinoma OR oral cavity cancer OR oropharynx cancer OR oropharyngeal cancer OR larynx cancer OR laryngeal cancer OR tongue cancer OR hypopharynx cancer).
Clinical studies that evaluated the association between IL-6 and HNSCC and which were published in English were reviewed. Two blinded investigators (GE, UU) assessed the quality of each study using a standardized set of eight predefined criteria adapted from Slim et al. [18]. Studies were classified as high, moderate or low quality according to their scores. Any disagreements in the selection of studies were resolved by consensus.
RESULTS
In total, 99 studies met the inclusion criteria for the systematic review. Unfortunately, the authors were not able to perform a meta-analysis due to the marked heterogeneity in the definition of HNSCC, the lack of a consistent study design, and the small sample sizes.
DISCUSSION
Serum IL-6 concentration and IL-6 expression in HNSCC
Currently, it is known that IL-6 plays a crucial role in immunoregulation and tumorigenesis. Therefore, IL-6 concentrations may increase in serum, saliva or at the tumor microenvironment of patients with HNSCC. Indeed, serum IL-6 concentrations were high in patients with HNSCC when compared with healthy controls [19]. On the other hand, Andersson et al. were unable to determine a statistically significant difference between plasma IL-6 concentrations in patients with HNSCC and healthy subjects [20]. In the literature, a variety of clinical studies have also reported higher serum IL-6 concentrations in patients with oral squamous cell carcinoma (OSCC) [21-23]. St John et al. [24] emphasized that serum IL-6 concentration might be used as a biomarker for OSCC (sensitivity, 57%; specificity, 100%). They also demonstrated that its sensitivity and specificity rates increased up to 99% and 90%, respectively, when serum IL-6 and saliva IL-8 concentrations were used concurrently. In addition, serum IL-6 concentrations were correlated with other inflammatory response biomarkers such as neutrophil-lymphocyte ratio and C-reactive protein levels in patients with OSCC [25]. Interestingly, Sotirovic et al. [26] were unable to demonstrate a significant difference between the serum IL-6 concentration of patients with laryngeal squamous cell carcinoma (LSCC) and control patients.
A clinical study, in which the relationships between health behaviors and pretreatment serum IL-6 concentrations of patients with HNSCC were evaluated, determined that current and former smoking status, poorer sleep scores, being older and higher tumor stage were significantly associated with higher serum IL-6 concentrations. However, alcohol intake, physical activity, body mass index, tumor location, race, education and income were not related to serum IL-6 concentrations in multivariate analysis [27]. On the other hand, Gao et al. [28] reported a correlation between history of alcohol consumption and IL-6 mRNA expression.
Human papilloma virus (HPV) 16 oncoproteins promote a proinflammatory cytokine “Oncostatin M” that promotes IL-6 expression; hence, viral oncoproteins induce IL-6 expression indirectly [29]. On the other hand, patients with HPV(+) had lower IL-6 concentrations than patients with HPV(–) [28]. The authors stated that HPV(+) cancer patients had better prognosis and the probable mechanism could be related to E6 and E7 oncoproteins that have significant effects on IL-6 regulation [28]. Moreover, Guerrera et al. [30] emphasized that IL-6 overexpression was particularly prominent at the HPV(–) tumor sites. Therefore, downregulation of IL-6 in HPV(+) patients with HNSCC might be associated with overexpressed cytokeratin proteins that may increase the sensitivity to radiochemotherapy.
IL-6 is a prognostic biomarker in HNSCC
Several studies have demonstrated the prognostic role of serum IL-6 concentrations and IL-6 overexpression in patients with HNSCC (Table 1). Serum IL-6 concentration was found to be an independent prognostic factor for overall- and disease free-survival in patients with OSCC [21]. In addition, longitudinal changes in serum IL-6 concentrations may also be used for the prediction of survival in patients with locally advanced oropharyngeal squamous cell carcinoma [31]. Serum IL-6 concentration was inversely correlated with overall- and progression free-survival in patients with LSCC [32]. Similarly, a significant association between high serum IL-6 concentrations and a decrease in treatment response and survival was reported in patients with HNSCC treated with radiochemotherapy [33]. Furthermore, Duffy et al. [34] emphasized that pretreatment serum IL-6 concentration might be a good biomarker for the prediction of recurrence and overall survival in patients with HNSCC.

Study characteristics and results of evaluating relation with survival parameters and serum IL-6 concentrations and expression in HNSCC
In the literature, the association between IL-6 overexpression and prognosis of patients with HNSCC has been demonstrated. Chen et al. [35] mentioned that IL-6 overexpression was associated with a significant decrease in survival of patients with pharyngeal squamous cell carcinoma. Similarly, several studies have reported that IL-6 expression was inversely related to prognosis and survival of patients with OSCC [28,36-38]. On the other hand, IL-6 expression was not associated with overall survival in patients with oropharyngeal SCC [39].
In HNSCC, the production of IL-6 from peripheral blood monocytes after lipopolysaccharide (LPS) stimulation was higher than control group [42]. In comparison with control and HNSCC cells, LPS stimulated monocyte IL-6 overexpression in vivo predicted poor survival in patients with HNSCC [40]. Moreover, high LPS induced monocyte IL-6 endotoxin responsiveness was determined to be an adverse prognostic factor irrespective of TNM stage [41]. IL-6 secreted from endothelial cells induced the HNSCC cells motility towards blood vessels and survival [43].
IL-6 overexpression generally portends dismal prognosis when combined with other biomarkers. In patients with oropharyngeal cancers, IL-6 and nuclear myoferlin (a member of the Ferlin family of proteins) overexpression had poorer survival rates (85% mortality rate) when compared with tumors which only overexpressed nuclear myoferlin [44]. In addition, oropharyngeal cancers which overexpressed both protein arginine methlytransferase-5 and IL-6 had poorer survival rates compared to oropharyngeal cancers which only overexpressed protein arginine methlytransferase-5 [45].
Salivary IL-6 concentrations in HNSCC
Salivary IL-6 concentrations have been particularly evaluated in patients with oral and oropharyngeal diseases. Several studies have reported that the salivary IL-6 concentration in patients with OSCC was higher than in healthy subjects [46-52]. Similarly, the salivary IL-6 concentration was significantly higher in patients with OSCC when compared to patients with premalignant lesions [51,53]. A clinical study showed that salivary IL-6 concentrations were significantly higher in patients with OSCC when compared with healthy subjects and patients with chronic oral inflammatory diseases such as chronic periodontitis or oral lichen planus [54]; therefore, the role of salivary IL-6 for early detection of OSCC was clearly demonstrated. Furthermore, Korostoff et al. [55] emphasized that salivary IL-6 might be used for tongue cancer screening. IL-6R salivary angiogenic protein was found in excessive amount in saliva of HNSCC patients; hence, authors stated that it might be used as a potential diagnostic biomarker [56].
Salivary IL-6 is a candidate biomarker for the monitoring of treatment response in OSCC [47]. A significant decrease in salivary IL-6 concentration was detected after successful treatment of patients with OSCC. In addition, post-treatment salivary IL-6 concentration was an independent risk factor for locoregional recurrence in OSCC. Therefore, it might be used as a biomarker for the diagnosis of early and late locoregional recurrence [57,58]. Arduino et al. [59] stated that salivary IL-6 was more highly expressed in patients with OSCC than in a control group, and higher salivary IL-6 concentrations were correlated with higher survival rates. In addition, Bossi et al. [60] compared the baseline and post-treatment salivary IL-6 concentrations in patients with HNC and treated with radio and chemotherapy, and demonstrated that posttreatment IL-6 saliva levels might be used as a biomarker for the prediction of oral mucositis and inflammatory processes after radio and chemotherapy.
Association between IL-6 and cancer cachexia in patients with HNSCC
Cancer cachexia, a complex pathophysiological process, is principally characterized by an impaired anabolism and increased catabolism which leads to muscle wasting and progressive functional impairment, and a decrease in quality of life in patients with HNSCC [61,62]. It is currently known that cancer cachexia is triggered by several inflammatory mediators and neuroendocrine responses [61-63]. Recently, the association between IL-6 and cachexia has been clearly demonstrated [63-65]. In experimental models, elevated IL-6 concentrations have been correlated with muscular atrophy, weight loss and hypophagia [66,67]. In an experimental oral cancer model, a specific angiotensin II receptor blocker (Telmisartan; Micardis, Boehringer Ingelheim, Ingelheim am Rhein, Germany), which also inhibits IL-6 expression, controlled cancer cachexia successfully when used in combination with cisplatin [68]. Similarly, Richey et al. [69] examined the association between several inflammatory mediators and cancer cachexia in patients with HNSCC and determined elevated serum IL-6 concentrations in patients with cachexia. However, a clinical study, which focused on the body composition of patients with HNSCC before and after radiochemotherapy, was unable to demonstrate a significant change in serum IL-6 concentration despite the development of cancer cachexia [70]. It is noteworthy that dietary pattern is likely to play a key role in serum IL-6 concentrations, and dietary supplementation with lycopene and carotenoid might reduce serum IL-6 concentrations in patients with HNSCC [71].
IL-6 gene polymorphism in different diseases of head and neck
IL-6 expression was found to be significantly higher in premalignant and malignant oral pathologies compared to healthy subjects [72]. Of note, IL-6 (–174) gene polymorphism was associated with oral premalignant lesions [73]. Moreover, IL-6 functional gene polymorphism (IL-6-174 G>C) had significant effects on the developmental risk of tobacco-related OSCC [74]. Although IL-6-174 G>C polymorphism was correlated with better survival in laryngopharyngeal cancers, IL-6-174 C/C had worse survival in oral cavity and hypopharyngeal cancer and better survival in LSCC [75]. A significant relationship between IL-6-174 gene polymorphism and OSCC was also reported [76]. Inflammation with IL-6 induction promoted tumorigenesis by altering global long interspersed nuclear element-1 hypomethylation in the oral cavity [77].
Serum IL-6 concentrations were higher in patients with OSCC than in healthy subjects and patients with premalignant lesions [21]. On the other hand, no statistically significant difference between patients with premalignant lesions and healthy individuals was determined. A study that evaluated the association of serum IL-6 concentrations in patients with leukoplakia and OSCC reported that IL-6 was not a good biomarker for the differential diagnosis of leukoplakia and OSCC. In addition, IL-6 expression was not different between oral premalignant and malignant lesions [72]. In contrast, Rhodus et al. reported that IL-6 concentrations increased significantly as the malignancy level increased when patients with OSCC, premalignant lesions (particularly lichen planus), and healthy cases compared [78]. Hence, the abovementioned data obviously indicate that higher salivary IL-6 concentrations are especially associated with malignant transformation of premalignant oral lesions.
IL-6 and tumor characteristics in HNSCC
IL-6 has a proliferative effect on the tumor microenvironment, and is likely to be associated with cancer progression, angiogenesis and metastases. Activation of the IL-6 signaling pathway induces aggressive cancer cell behavior such as higher tumor growth and invasion rate [35]. IL-6 overexpression was associated with the pattern of invasion, vascular invasion and pathological nodal status [36]. Therefore, IL-6 targeted therapies seem to be promising for the cessation of tumor growth and reducing tumor volume. Anti-IL-6 therapy might provide a decrease in endothelial cells, tubule formation and neoangiogenesis by blocking the autocrine growth mechanism [79]. IL-6 may induce antiapoptotic factors by activation of signal transducer and activator of transcription 3 (STAT3) and suppress cisplatin-induced apoptosis. In fact, IL-6 overexpression may indicate a low rate of treatment response in patients with OSCC treated with radiochemotherapy [37]. OSCC are not the only cells able to produce IL-6. Fibroblastic cells are also able to express IL-6 which might be one of the major mechanisms of bone destruction in patients with OSCC [80]. In addition, IL-6 and hepatocyte growth factor had a synergistic effect on tumor migration and invasion in HPV-negative oropharyngeal cancer cell lines [81].
Serum IL-6 also plays an important role in the progression of HNSCC. Elevated IL-6 levels were associated with tumor size and nodal metastasis in patients with OSCC [82]. In other study, elevated levels of IL-6 were related with higher T-stage, pathological stage, bone invasion and tumor depths in patients with OSCC [21]. Serum IL-6 concentrations were high in patients with T3/T4-stage, positive nodal metastases and advanced stage HNSCC [19,83,84]. Moreover, serum IL-6 concentrations were correlated with tumor stage and were higher in patients with stage IV HNSCC when compared with patients with stage I-III HNSCC [85]. They were positively correlated with tumor pathological stage such as grade, depth, activity, and invasiveness [86]. They were also correlated with local control and were an important indicator of radiotherapy responses in patients with HNSCC [33]. A clinical study in which 399 patients with HNSCC were evaluated showed that IL-6 overexpression indicated cisplatin resistance and was associated with poor prognosis [28]. Furthermore serum IL-6 might be a potential predictive biomarker for resistance to dasatinib-cetuximab in patients with HNSCC [87]. In addition, blocking ERK dependent IL-6 signaling pathway enhanced the sensitivity to Buparlisib (PI3K inhibitor) in HNSCC patients [88]. Serum IL-6 was shown to be an independent risk factor for recurrence in OSCC [89]. Moreover, circulating IL-6 was a potent predictor of second primary cancer in patients with HNSCC [90].
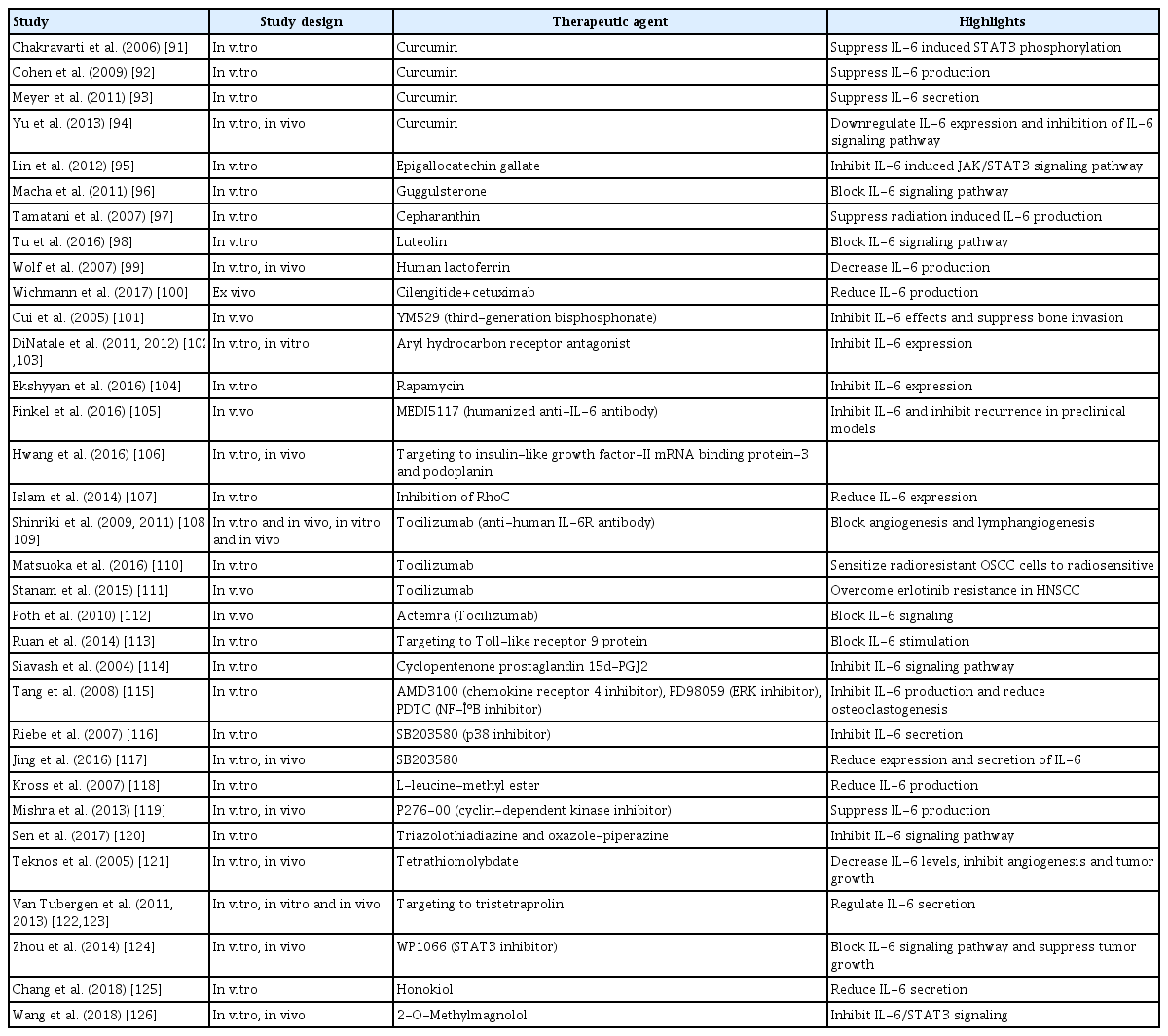
IL-6: a promising target for the treatment of HNSCC
Novel therapeutic agents, which are specifically targeted to inhibit IL-6 mediated inflammation, are promising candidates for the treatment of HNSCC (Table 2) [91-126]. Moreover, endothelium secreted IL-6 and IL-6R promote self-renewal and survival of cancer stem-like cells. Therefore, inhibition of the IL-6 signaling pathway may also reduce the fraction of cancer stemlike cells in HNSCC [127].
CONCLUSION
To the best of our knowledge, this is the first systematic review in which the role of IL-6 and its signaling pathway in HNSCC has been comprehensively evaluated. It is clear that IL-6 plays several key roles in different aspects of HNSCC such as carcinogenesis, progression, invasiveness, angiogenesis and metastasis. The IL-6 signaling pathway may also be related to cancer cachexia and may predict treatment response. Moreover, serum IL-6 concentrations and IL-6 expression are candidate prognostic biomarkers. IL-6 targeted therapies are promising and may be added to the armamentarium of HNSCC therapeutics in the near future. However, prospective, well-designed, and appropriately analyzed large-scale clinical studies are required.
HIGHLIGHTS
▪ Interleukin-6 (IL-6) has several effects on inflammation and carcinogenesis and regulates the immune system.
▪ IL-6 is a candidate prognostic biomarker in patients with head and neck squamous cell carcinoma.
▪ IL-6 is correlated with aggressive and invasive tumor type.
▪ IL-6 targeted therapies are promising treatment modalities for patients with head and neck cancer.
Notes
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Visualization, Writing–original draft, review, & editing: all authors.