Comparative Study of Gasless Transaxillary, Bilateral Axillo-Breast, Unilateral Axillo-Breast With Carbon Dioxide Insufflation, Retroauricular, and Transoral Vestibular Endoscopic Thyroidectomy Approaches at a Single Institution: A Retrospective Analysis and Lessons Learned
Article information
Abstract
Objectives
This study aimed to present our experiences with various approaches for endoscopic thyroidectomy (ET) and to offer lessons for choosing an approach.
Methods
The medical records of 701 patients who underwent ET via the transaxillary (TA), bilateral axillo-breast (BABA), unilateral axillo-breast with carbon dioxide insufflation (UABA), retroauricular (RA), or transoral vestibular (TO) approach between May 2008 and March 2020 were retrospectively reviewed. Postoperative pain and cosmetic outcomes were evaluated using visual analog scales.
Results
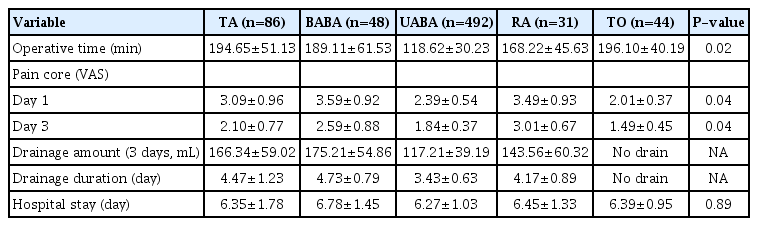
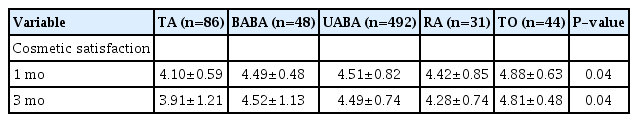
The mean operative time of UABA was the shortest among the five approaches (TA, 194.65±51.13 minutes; BABA, 189.11±61.53 minutes; UABA, 118.62±30.23 minutes; RA, 168.22±45.63 minutes; TO, 196.10±40.19 minutes; P=0.02). BABA was the most painful approach, while TO was the least painful on postoperative day 1 (TA, 3.09±0.96; BABA, 3.59±0.92; UABA, 2.39±0.54; RA, 3.49±0.93; TO, 2.01±0.37; P=0.04) and day 3 (TA, 2.10±0.77; BABA, 2.59±0.88; UABA, 1.84±0.37; RA, 3.01±0.67; TO, 1.49±0.45; P=0.04). The TO group had the best cosmetic outcomes at 3 months (TA, 3.91±1.21; BABA, 4.52±1.13; UABA, 4.49±0.74; RA, 4.28±0.74; TO, 4.81±0.48; P=0.04).
Conclusion
We present a single-surgeon experience of five distinctive ET approaches and the lessons from each approach, together with a literature review. This data may aid endoscopic thyroid surgeons in choosing from various ET approaches.
INTRODUCTION
Various remote endoscopic thyroidectomy (ET) approaches have been developed to avoid anterior neck scarring. These include the transaxillary (TA), chest, breast, retroauricular (RA), and transoral (TO) approaches [1-6]. These newly conceptualized techniques were devised to cope with the limitations of previous approaches. For example, the RA approach was developed to overcome the invasiveness of the large flap elevation in the TA and bilateral axillo-breast (BABA) approaches, and the TO approach was introduced as part of the emerging concept of natural orifice transluminal endoscopic surgery that seeks not to leave any scars on the skin [6,7]. From a practical standpoint, it is difficult for a surgeon to adopt and practice all approaches that have been developed by other surgeons due to limitations such as finite time and financial support, as well as the substantial amount of physical and mental labor that would be required to do so. Therefore, reports to date have only compared two or three approaches at a time.
However, we believe that each approach has its own characteristics, advantages and disadvantages compared to others, and that it is worthwhile to try and experience as many new approaches as possible, however difficult it may be to find a suitable approach for a specific case and to develop new approaches since the early 2000s. We started ET in 2008 and performed it in over 700 cases through 2020, using the TA, BABA, unilateral axillo-breast with carbon dioxide insufflation (UABA), RA, and TO vestibular approaches to ET [1,2,4-6]. This study aimed to present and compare the outcomes of each approach, and to describe the lessons learned from these experiences.
MATERIALS AND METHODS
The Institutional Review Board of the Korea Cancer Center Hospital approved this retrospective study (No. 2021-08-003). Informed consent was obtained from all patients regarding the surgical approaches and possible complications.
The medical records of 701 patients who underwent endoscopic hemithyroidectomy with or without central lymph node dissection via a TA, BABA, UABA, RA, or TO approach at the Department of Otorhinolaryngology-Head and Neck Surgery, Korea Cancer Center Hospital from May 2008 to March 2020 were analyzed. The center performed 86 cases of TA since 2008, 48 cases of BABA since 2009, 492 cases of UABA since 2011, 31 cases of RA since 2014, and 44 cases of TO since 2018. All cases were performed by a high-volume single surgeon (MCL). Central lymph node dissection was performed in all the malignant cases. Surgical approaches available at the time of operation were clearly explained, and the patients freely chose their preferred technique. During counseling, the medical and surgical history, job, and preferences of the patients were thoroughly checked considering their impact on each surgical approach. For example, the TO approach was not recommended for patients who underwent mandibular surgery, such as chin augmentation or maxillomandibular advancement.
The inclusion criteria for endoscopic hemithyroidectomy were as follows: thyroid differentiated carcinoma with low risk (unilateral, single, size ≤2 cm, no prior radiation to the neck, clinically no regional and distant metastases, as well as no aggressive variants), and benign tumor (adenomatous goiter and follicular neoplasm) less than 6 cm in size. The exclusion criteria included benign or malignant tumors larger than 6 cm, severe underlying thyroiditis, unfavorable thyroid lobe shapes such as a substernal extension or a high set upper pole, unfavorable pathologic states such as poorly or undifferentiated thyroid cancer, extensive nodal metastasis, extrathyroidal extension, and local invasion to nearby structures, as well as combined neck procedure needed (lateral neck dissection, lymph node biopsy in the lateral neck).
Preoperative patient workup included a blood test, physical examination, laryngoscopy, ultrasonography with fine-needle aspiration and cytologic evaluation, and high-resolution computed tomography of the whole neck. Data from patient medical records and the thyroid cancer database which was established to facilitate clinical research were collected. The data analyzed in this study were patient age, sex ratio, body mass index, pathology, tumor size, operation time (cut-suture time), extent of surgery, visual analog scale (VAS) of pain score and cosmetic satisfaction, amount of drainage, and postoperative complications (vocal cord palsy, infection, bleeding, sensory deficit, lip asymmetry, and tracheal injury).
Operative techniques
Surgeries were performed using the previously described endoscopic approaches. The detailed surgical technique per approach was reported in several studies; TA was described by Koh et al. [1], BABA by Choe et al. [2], UABA by Lee et al. [4], RA by Terris et al. [5], and TO by Anuwong [6]. The drawings by professional medical illustrator show schemas of each approach (Fig. 1).
Outcome evaluation
The operative time was from skin incision to closure. Postoperative pain on days 1 and 3 was assessed using the VAS, with scores ranging from 1 (no pain) to 5 (severe pain). Drainage amounts were measured daily, and the sum of the amounts of the first three consecutive days was used for comparison. Negative drainage was maintained until the 1-day amount was reduced to below 25 mL/day if applied postoperatively. Laryngoscopic examination was performed on postoperative day 1, and patients with vocal cord paralysis were re-examined at 1, 3, and 6 months. Recurrent laryngeal nerve paralysis was regarded as temporary if vocal cord movement recovered within 6 months. We prospectively evaluated postoperative subjective cosmetic satisfaction via questionnaires using VAS scores at 1 and 3 months postoperatively. The VAS score for subjective cosmetic perception ranged from 1 to 5 (very dissatisfied to very satisfied).
Statistical analysis
All statistical analyses were performed using one-way analysis of variance, Kruskal-Wallis H test, and chi-square test on SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at P<0.05.
RESULTS
The clinicopathological characteristics of the patients are summarized in Table 1. Age, sex ratio, body mass index, pathology, and tumor size were not significantly different among the patient groups. Regarding patients’ past surgical history, two patients who received mandible surgery for cosmetic purposes and requested TO for papillary thyroid carcinoma underwent ET via UABA. Three patients whose jobs were in entertainment wanted TA or RA but underwent TO due to cosmetic issues such as an axillary or retro-auricular scar. Of the three patients who previously underwent breast augmentation surgery for cosmetic purposes, one underwent RA and the others underwent TO. Two patients with a prior history of mastectomy for breast cancer underwent TO for thyroid cancer.
The surgical outcomes are shown in Table 2. The operative times (TA, 194.65±51.13 minutes; BABA, 189.11±61.53 minutes; UABA, 118.62±30.23 minutes; RA, 168.22±45.63 minutes; TO, 196.10±40.19 minutes; P=0.02) of each approach were significantly different. UABA was the shortest of the five approaches. The VAS scores for pain at postoperative day 1 (TA, 3.09±0.96; BABA, 3.59±0.92; UABA, 2.39±0.54; RA, 3.49±0.93; TO, 2.01±0.37) and day 3 (TA, 2.10±0.77; BABA, 2.59±0.88; UABA, 1.84±0.37; RA, 3.01±0.67; TO, 1.49±0.45) showed significant differences (both P=0.04). Among the five approaches, BABA was the most painful, and TO was the least painful. The total amount of drainage for the first 3 days could not be compared because drainage was not applied for TO. However, UABA showed the least amount of drainage among the four groups in which the negative drainage was applied, reflecting a statistically significant difference (TA, 166.34±59.02 mL; BABA, 175.21±54.86 mL; UABA, 117.21±39.19 mL; RA, 143.56±60.32 mL; P=0.03). The duration of drainage showed a pattern similar to that of the amount of drainage. The duration of hospital stay was not significantly different among the five groups (TA, 6.35±1.78 days; BABA, 6.78±1.45 days; UABA, 6.27±1.03 days; RA, 6.45±1.33 days; TO, 6.39±0.95 days; P=0.89).
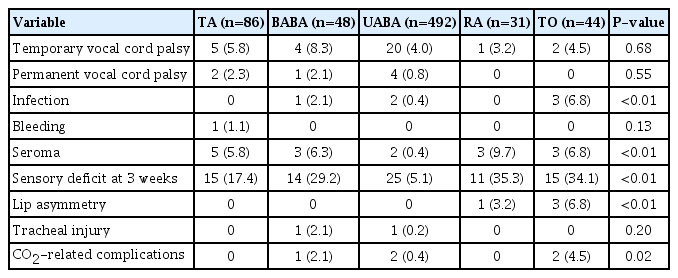
Postoperative complications are compared in Table 3. Temporary (3.2%–8.3%) and permanent vocal cord palsy (0%–2.3%) were identified in our study. There were no significant differences among the five groups in terms of vocal cord palsy. Infections took place in one case (2.1%) of BABA, two cases (0.4%) of UABA, and three cases (6.8%) of TO. A significant difference was observed (P<0.01). Seroma occurred in five cases (5.8%) of TA, three cases (6.3%) of BABA, two cases (0.4%) of UABA, three cases (9.7%) of RA, and three cases (6.8%) of TO. Seroma occurrence showed a significant difference across groups (P<0.01). Sensory deficits in the involved area at postoperative week 3 were identified in 15 cases (17.4%) of TA, 14 cases (29.2%) of BABA, 25 cases (5.1%) of UABA, 11 cases (35.3%) of RA, and 15 cases (34.1%) of TO, with a significant difference (P<0.01). Lip asymmetry was found in one patient (3.2%) who underwent RA and four (9.1%) who underwent TO, which constituted a significant difference (P<0.01). Postoperative bleeding and intraoperative tracheal injury were observed. CO2-related complications (hypercapnia and mild gas embolism) occurred in one (2.0%) case of BABA and in two cases (4.5%) of TO, reflecting a significant difference (P=0.02). The cosmetic satisfaction scores showed significant differences between the study groups, and the TO group had the highest satisfaction scores at postoperative day 1 (P=0.04) and 3 months (P=0.04) (Table 4).
DISCUSSION
The present study documented our various experiences with five distinctive endoscopic approaches for thyroidectomy (TA, BABA, UABA, RA, and TO) and compared the surgical outcomes of each technique. In recent years, many types of endoscopic approaches for thyroidectomy have gained popularity. Surgeons who developed new techniques or adopted previous endoscopic approaches have argued that these new approaches have many advantages, including cosmesis of the anterior neck and reduced postoperative pain and discomfort. However, some have reported that these approaches are more invasive and remote than conventional open approaches [8-10]. After performing the TA and BABA approaches, we came to believe that the balance between invasiveness and cosmesis was most important. To cope with the limitations of TA and BABA, especially in terms of invasiveness, in 2012, we devised our own UABA, which showed less postoperative pain, drainage amount, and good cosmesis [4]. Thereafter, we adopted RA in 2014 and TO in 2018 to determine which ET approach would achieve the best balance between invasiveness and cosmesis. During all these experiences of ET, we have thoroughly examined the characteristics of each approach, including the invasiveness and cosmesis, as well as other advantages and disadvantages, with the aim of choosing a proper approach for each case. Unlike previous studies comparing only two or three endoscopic approaches, this work described our experiences with and compared the outcomes of the five most popular approaches to ET in procedures performed at a single institution. To the best of our knowledge, this work is the first report that describes and compares these most popular approaches in procedures performed by a single surgeon at a single institution.
To evaluate and compare the invasiveness of each approach, we measured surgical outcomes such as operative time, postoperative pain score, and drainage amount and duration (Table 2). We included only hemithyroidectomy cases in this study to facilitate an exact comparison. UABA showed the shortest operative time. Although there were discrepancies in the number of cases for each approach, we think that this result is explained by the fact that UABA does not necessitate elevating a large working space from the axilla and areola to the operation field through gas insufflation. Nonetheless, it is also clear that the overwhelmingly predominant number of UABA cases, in contrast to the relatively low case numbers for BABA, RA (with a case number below the previously reported learning curve), and TO, also affected this outcome. Patients who underwent TO showed the lowest pain score on postoperative days 1 and 3. Although we could not quantify the exact area or volume of the surgical field, the dissection length and area from the incision site of the oral mucosa to thyroid gland are definitely the smallest in the TO approach [6]. We speculate that less dissection may have resulted in less tissue damage, which in turn caused less postoperative pain. The drainage amount and drainage duration could not be compared among all five approaches because we did not apply negative drainage in the TO approach, as previously described by Anuwong [6]. Since it was associated with the lowest pain scores and no postoperative drainage, TO showed the best results from the standpoint of invasiveness.
In terms of complications, the incidence of temporary and permanent vocal cord palsy did not differ significantly among the five approaches. The rates of temporary (4.0%–8.3%) and permanent vocal cord palsy (0%–2.3%) in our series were not substantially different from those reported in previous studies [11]. In this study, vocal cord palsy was more frequent in the early period of practice of each approach. With more experience, we expect that the rate will decrease over time. Wound infection was very rare except for in the TO approach because all four non-TO approaches are, by definition, clean surgery like the conventional open thyroidectomy. On the contrary, TO is a type of clean/contaminated surgery, and the infection rate was 6.8% in this study [12]. This rate is much higher than reported in previous studies, including a meta-analysis that presented very low rates of 0.1% to 1% [13]. However, some other researchers have reported a higher rate of surgical site infections, in 6%–7.4% of TO patients [11]. We speculate that heterogeneity in the definitions of surgical site infection in previous research may account for this difference. We included all the cases of postoperative infection, including those showing mild erythema, tenderness, or swelling. Two of our infection cases resolved after prolonged antibiotic treatment; however, one case that showed abscess formation needed aspiration and intravenous antibiotic treatment. Preoperative and postoperative antibiotics, antiseptic skill and instrument handling, and meticulous removal of blood clots, char from vessel coagulation, and other debris through irrigation are necessary to prevent infections, especially in TO.
Seroma occurred in 0.4%–9.7% of patients in our series. Most cases were not severe and occurred when compression was not applied. After we started applying a compressive dressing with an elastic bandage or a surgical bra for 2 or 3 days, seroma no longer occurred. All cases resolved after one or two instances of aspiration and compression. Sensory deficit at postoperative 3 weeks was observed in 5.1%–35.3% of patients in our series. It is certain that more extensive tissue damage occurs in ET than in conventional open thyroidectomy. Contrary to TA, BABA, UABA, and RA, which present a broad area of sensory deficit over the chest and neck, the numbness after TO typically occurred in areas innervated by the mental nerve. This has been well documented in other studies, with reported rates ranging from 0% to 100% [14,15]. The wide range of reported rates derives from the heterogeneity of the definition of mental nerve injury. Fortunately, in our series, sensory deficit usually subsided in a few months, but in one case, it did not disappear completely even after 1 year. Special care should be taken not to damage the mental nerve branches when two lateral vestibular ports are inserted [6].
Lip asymmetry was found in four cases. In one case of RA, it occurred as a result of indirect thermal damage by monopolar cautery or the energy device to the marginal mandibular nerve during flap elevation around the mandible angle. It subsided in several months. Meticulous dissection is necessary when a surgeon elevates a flap around the mandible angle. Three TO cases developed a temporary asymmetry in the mouth corner (Fig. 2). To the best of our knowledge, no previous report has described this subtle asymmetry in the mouth corner. We assume that this derived from the asymmetric force of scar contracture during the healing stage. It resolved in 1 to 2 months without any sequelae. Nonetheless, even a subtle asymmetry of this type can pose a problem for some sensitive patients, so it is important to assure them that this phenomenon has a good prognosis.

Lip asymmetry shown after the transoral endoscopic thyroidectomy vestibular approach at postoperative 1 month in each affected patient (A, B).
CO2-related complications (hypercapnia and mild gas embolism) occurred in 5 cases in BABA, UABA, and TO using CO2 gas. Even though these complications were successfully controlled intraoperatively, they can be dangerous. Surgeons should be cautious in monitoring vital signs, including pCO2 levels, and should not expose the lumen of large veins while performing an endoscopic approach with CO2 insufflation. If CO2 embolism is suspected during an operation, CO2 insufflation should be stopped, 100% oxygen should be administered, the patient should be placed in the left lateral decubitus and reverse Trendelenburg position, hyperventilation should be performed, and if necessary, cardiac resuscitation should be done quickly [16]. Among the five approaches, TO was significantly best in terms of cosmetic satisfaction (Table 4). TO does not require a skin incision that could be visible. On the contrary, TA and RA, which leave a long axillary or retroauricular scar, showed somewhat lower satisfaction scores at postoperative 3 months.
Below we present brief descriptions and lessons learned, including the advantages and disadvantages, for each of the five approaches based on our experiences and a review of the literature. TA requires a long and large flap from the axilla to the thyroid; therefore, the surgical view and instrument handling are excellent [1]. It is very straightforward to learn and easy to perform for novice surgeons. Furthermore, TA has strong advantages when meticulous dissection of the upper pole or Berry’s ligament is needed because the surgical view and instrument direction are from the lateral to medial aspects, as in the open approach. However, TA results in severe pain and dysesthesia around the chest, as well as a large amount of drainage due to its invasiveness [17]. Moreover, the strong retraction needed to maintain the working space for a long operation time may lead to damage on the edge of the incision and result in a poor axillary incision scar [18]. Seroma from severe tissue damage during a long operation occurred in 5.8% of cases (Table 3). After the development of many alternative techniques, TA has not been performed frequently. Nevertheless, it is especially useful for the easy removal of large thyroid lobes or tumors exceeding 4 cm because it offers a large working space and a long vertical incision in the axilla [19]. However, TA is not an ideal procedure for patients who require or prefer no scars in the axilla due to their jobs.
BABA uses CO2 gas to make and maintain the working space, since it entails a large flap elevation even though the incision scars are very small [2]. The cosmetic outcomes are excellent; however, the large working space sometimes leads to complaints of chest pain, discomfort, and adhesion [17]. Although BABA offers good operative vision, it requires a learning curve [20]. Since endoscopic instruments approach from the contralateral side over the trachea, the dissection around the upper pole and Berry’s ligament is frequently complicated. BABA is useful when the surgeon performs total thyroidectomy because it symmetrically approaches each thyroid lobe in the same working space [21]. Conversely, it may be criticized because lobectomy should be performed in the same working space as needed for total thyroidectomy. Because working space and the flap are rather large compared to the conventional open approach, BABA is not used as frequently.
UABA was developed by the corresponding author of this study to address the limitations of TA and BABA [4]. It uses three trocars with CO2 gas insufflation to approach the thyroid gland without an axillary vertical long incision (Fig. 1). The operative time is shorter, postoperative pain and discomfort are less intense, and the drainage amount is lower because UABA does not involve the elevation of a long and large flap like that in TA [22]. The operative vision and instrument handling are as excellent as that of TA; therefore, dissection around the upper pole or Berry’s ligament is easy. The cosmetic results are good because UABA only leaves two small scars in the axilla and one small scar in the periareolar area. UABA and a modification of UABA using a robot system, called the transaxillary gas-insufflation approach, has been performed at some thyroid centers, with good overall patient satisfaction [22,23].
RA has several advantages over TA or BABA because it uses a shorter path to the thyroid, via a retroauricular incision, than approaches through the axilla or chest [5]. It does not cause chest discomfort or brachial plexus injury, which were reported as early complications of TA [10]. Otolaryngologists have a relative strength in this approach compared to general surgeons since they are neck anatomy experts. The endoscopic view and instrumentation are good, and the dissection around the upper pole and Berry’s ligament is excellent because of the oblique (lateral superior to medial inferior direction) approach angle. However, the inevitable cervical sensory nerve damage during flap elevation causes pain or dysesthesia above the involved neck area. Moreover, the incision scar can sometimes be disfiguring due to the long-term retraction damage to the incisional edge along the posterior hairline [18]. In addition, seroma occurred in 9.7% of cases in our series (Table 3). RA is especially useful when the tumor or thyroid is large because it makes a long incision and elevates a large flap. It is also helpful when a combined neck procedure, such as neck biopsy or dissection, is necessary [24]. At our institution, we performed three cases of total thyroidectomy with lateral neck dissection and two cases of thyroid lobectomy with lateral neck lymph node biopsy via RA (one in a confirmed case of tuberculosis and one in a case of lymph node hyperplasia) that were not included in this study.
TO is the most recent and popular approach, and it is cosmetically ideal since it leaves no scars on the skin [6,25]. Above all, it has the shortest length from the mucosal incision site to the thyroid. In addition, both thyroid lobes can be dissected in the same working space, so total thyroidectomy or isthmectomy are easily performed [26]. Moreover, central neck dissection can be performed without difficulty because of the surgical view it provides from the superior to inferior aspects. However, it may be difficult to dissect the upper pole or Berry’s ligament due to the acute approaching angle of the instrument in this region. At least one instrument should cross over the trachea or cricoid cartilage; hence, the surgeon should be careful not to tear the capsule of the thyroid or crush the tumor when it is located in the upper pole or near Berry’s ligament [27]. Nodule size is also important. If a nodule is large (benign >6 cm, malignant >2 cm), it is difficult to operate and extract the specimen through a mucosal incisional site via TO [27]. Among the complications, there were some cases of infections that might have originated from the oral cavity incision site (Table 3). The most notable complications were lip and chin numbness [11]. We assume that the numbness was inevitable due to the traction injury to the mental nerve; however, in our experience, this numbness is beneficial since it masks the postoperative pain around the lip and chin in the early postoperative period. As a result, TO had the lowest pain scores. CO2-related complications (hypercapnia and mild gas embolism) occurred in two cases (4.5%), although they were successfully controlled intraoperatively. Surgeons should be cautious in monitoring vital signs, including pCO2 levels, and should not expose the lumen of large veins during the CO2 insufflation endoscopic approach [11,16]. The gasless transoral ET vestibular approach was recently introduced, and it offers a clear surgical view with efficient fume removal and no risk of CO2 gas-related complications [28]. We have no experience with that approach, but it seems to be more invasive than conventional TO, which uses CO2 insufflation, because it uses a specific retractor to maintain a working space. Each of the five most common remote access thyroidectomies described has its own characteristics and limitations [17,29-33]. Hence, it is difficult to choose which approach is best for each patient with a thyroid nodule planned for endoscopic removal. We believe that the comparative analysis and the lessons we presented may help endoscopic surgeons choose an appropriate approach.
This study has several limitations. First, there was a considerable discrepancy in the number of cases in this study. This means that all of the surgical outcomes, including operative time, drainage, pain, and complications, could have been biased in several ways. Ideally, it would be best to collect and compare data for each approach only after the learning curve. However, it is impossible to do so for procedures performed by a single surgeon at a single institution in the real world. Various reports have described the learning curve of each approach (endoscopic or robotic) as 7–60 cases [12,20,32,34,35]. In our series, TA (86 cases vs. previously reported learning curve of 30–60), BABA (48 cases in our series vs. previous reports of 30–35), UABA (492 cases in our series; although no previous report has described the learning curve, this number is clearly high enough), and TO (44 cases in our series vs. previous reports of 7–11) were performed at volumes exceeding the learning curve. Only for RA (31 cases in our series vs. previous reports of 50) was the number of cases in our series less than the learning curve reported previously. Although our numbers of cases are not sufficient for an absolutely exact comparison, we also believe that the data may be valuable because all the operations were performed by a single surgeon in a homogenous surgical setting at a single institution. Further studies involving more cases will be necessary to address this issue.
Second, total thyroidectomy cases were not included. Although the completeness of thyroidectomy and parathyroid preservation can only be determined in total thyroidectomy cases, the authors usually performed ET when cases were suitable for thyroid lobectomy. If total thyroidectomy was indicated, the conventional open approach was recommended. Based on our experience, we believe that ET is still not completely appropriate for total thyroidectomy in terms of invasiveness (long operation time, tissue damage, accompanying pain or dysesthesia felt on the overlying skin, and possible complications, as previously described), parathyroid preservation, as well as the level of lymph node dissection.
Third, we only used the VAS scale for assessing and comparing cosmetic outcomes. We started performing TA in 2008. Unfortunately, we have used a simple crude VAS score to assess cosmetic satisfaction throughout this period, which necessitated the use of the VAS for comparisons in this study. Nonetheless, we acknowledge the importance of using a validated questionnaire such as the Vancouver scar scale [36]. In future research, we will consider this methodological point.
Finally, experiences of performing robotic surgery are not included in this study. There is a wealth of studies describing the superiority of the robotic approach [34]. A robotic system provides a magnified stereoscopic surgical view, a flexible instrument like a wrist, tremor filtering, and motion scaling. Moreover, newer single-port robotic systems have been developed and are changing the landscape of the remote approach [37]. We recently tried to use a robotic system for our own UABA with gas insufflation, but we still perform ET. Historically, the endoscopic approach always preceded the corresponding robotic approach. We think ET is still meaningful and necessary in terms of cost-effectiveness, the lower complexity of instrument changes and handling, the development of new approaches, and the role of adjunctive procedures and testbeds for robotic application.
In conclusion, we presented a comparative analysis of five distinctive ET approaches and discussed the lessons for each approach from our experiences and a literature review. This work may aid endoscopic thyroid surgeons to choose among various approaches.
HIGHLIGHTS
▪ This is the first single-center study to compare experiences with the five most popular approaches for endoscopic thyroidectomy.
▪ Each endoscopic approach has its own characteristics and limitations.
▪ This comparative analysis and the lessons learned from our experiences may help endoscopic surgeons choose an appropriate approach.
Notes
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: MCL. Data curation: JA, IJC. Formal analysis: JA. Methodology: JA, IJC. Visualization: BCL, JR. Writing–original drift: MCL. Writing–review & editing: MCL, BCL.