The Surgical Outcome of Endoscopic Dacryocystorhinostomy According to the Obstruction Levels of Lacrimal Drainage System
Article information
Abstract
Objectives
Many factors influence the outcome of endoscopic dacryocystorhinostomy (DCR). One of the most important prognostic factors is the level of obstruction in the lacrimal drainage system. The main objective of this report is to evaluate both the frequency of obstruction by anatomical region of the lacrimal drainage system on dacryocystography (DCG) and the surgical outcome of endoscopic DCR according to the obstruction level.
Methods
A retrospective series of 48 patients (60 eyes) who had undergone endoscopic DCR from January 2005 to November 2007 were enrolled. Preoperative evaluation consisted of a standard examination which included lacrimal irrigation, probing, DCG and osteomeatal unit (OMU) computed tomography. Patients were classified into four groups according to the obstruction level on DCG. Surgical outcome was evaluated postoperatively by subjective improvement of epiphora and patent rhinostomy opening on nasal endoscopic exam.
Results
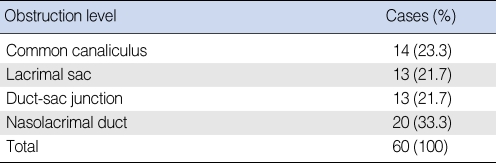
Of 60 eyes, the levels of obstruction were the common canaliculus in 14 eyes (23.3%), the lacrimal sac in 13 eyes (21.7%), the duct-sac junction in 13 eyes (21.7%) and the nasolacrimal duct (NLD) in 20 eyes (33.3%). The ductsac junction obstruction was treated most successfully (100%), followed by NLD obstruction (90%), common canaliculus obstruction (78.6%) and saccal obstruction (69.2%).
Conclusion
In patients with lacrimal drainage system obstruction, preoperative evaluation of obstruction level using DCG may be helpful for predicting the surgical outcome of endoscopic DCR. The saccal obstruction may have a worse prognosis than the other obstruction levels.
INTRODUCTION
Acquired lacrimal drainage system obstruction is a common ophthalmic problem and accounts for 3% of ambulatory clinic visits (1). It is caused by recurrent inflammation, facial trauma, tumor, etc. There are many clinical tests to evaluate the lacrimal drainage system, but it is difficult to identify the exact level of the obstruction. Dacryocystography (DCG) is a practical method to determine the exact obstruction level.
Since its first description by McDonough and Meiring (2) 20 yr ago, endoscopic dacryocystorhinostomy (DCR) has been gaining popularity due to technological advances in endoscopes and other modern instruments of rhinologic surgery (3). According to the definition of success in previous studies, the success rate of endoscopic DCR ranged from 70% to 95% (4-7).
Many factors influence the outcome of endoscopic DCR, and one of the most important prognostic factors determining success rate is the obstruction level in the lacrimal drainage system (8-10). But so far, there are few reports which analyse success rate according to the obstruction level.
Therefore, the aim of this report is to determine the frequency of lacrimal drainage system obstruction in different anatomical levels using DCG and to evaluate the surgical outcome of endoscopic DCR according to the obstruction level.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of sixty eyes of 48 patients (8 males and 40 females) who had undergone endoscopic endonasal DCR from January 2005 to November 2007.
All patients were evaluated by an ophthalmologist before surgery using lacrimal probing, lacrimal irrigation, Jones' test, and DCG. The need for additional nasal surgery (e.g., septoplasty, sinus surgery) was also determined preoperatively by nasal endoscopic exam and osteomeatal unit (OMU) computed tomography.
Patients with previous history of facial bone fracture, surgery on lacrimal drainage system or functional obstructions were excluded.
Patients were classified into four groups according to the obstruction level determined by DCG (Fig. 1): 1) obstruction of common canaliculus, 2) obstruction of lacrimal sac, 3) obstruction of duct-sac junction, 4) obstruction of nasolacrimal duct (NLD). The lacrimal sac obstructions presented as a filling defect and/or severe stenosis of the sac on DCG.
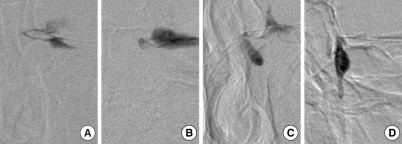
Preoperative dacryocystographic findings show various obstruction locations in the left lacrimal drainage system (A) common canaliculus. (B) lacrimal sac. (C) duct-sac junction. (D) nasolacrimal duct.
Surgical outcome was evaluated postoperatively by subjective improvement of epiphora and the patency of neo-ostium of endoscopic DCR on nasal endoscopy. We defined a successful outcome as a marked improvement of preoperative epiphora and a patent neo-ostium on nasal endoscopic exam. Statistical analyses were conducted using the SPSS ver. 12.0. Fisher's exact test was used to compare the success rate between the groups. P<0.05 was regarded statistically significant.
Operative techniques
Endoscopic DCR is performed under general anesthesia. The patient is placed in a supine position with the head elevated 15 degrees. After shrinkage of the nasal mucosa with a packing gauze soaked in a mixture of 1:200,000 epinephrine and 2% lidocaine, the mucosa surrounding the lacrimal sac is infiltrated with the same solution. A 4 mm diameter, zero or thirty degree endoscope is used. Using a slit knife (SatinSlit™, 2.75 mm, angled, Alcon Co., Cleveland, OH, USA), a vertical mucosal incision is made 8 mm anterior from the attachment of uncinate process at the lateral nasal wall and it is extended from just above the anterior attachment of the middle turbinate to the attachment of the inferior turbinate (Fig. 2A).

Operative technique of endoscopic dacryocystorhinostomy. (A) A vertical mucosal incision is made at the lateral nasal wall. (B) Mucosal flap is elevated and resected. (C) The maxillary bone covering the lacrimal sac is removed. (D) The anteriorly based lacrimal sac flap is everted and adjusted to accurately appose the nasal mucosa. Note that the common canalicular opening (indicated with arrow) is visible. (E) The silicone bicanalicular tube is positioned. (F) Nasal endoscopic finding six months after surgery. The rhinostomy opening (arrow) is wide and patent. S: septum; MT: middle turbinate; IT: inferior turbinate; LS: lacrimal sac.
The mucosal flap is elevated backwards off the maxillary bone and removed with cutting forceps (Fig. 2B). Bone covering the lacrimal sac is then gently removed with rongeurs (Koros® Osteo-Punch Rongeurs™, 2 mm, T. Koros Surgical Instruments Corp, Moorpark, CA, USA) and diamond DCR bur (High Speed Diamond DCR Bur®, 2.5 mm, 20 degree curved, Medtronic Xomed, Inc, Jacksonville, FL, USA) until the sac is widely exposed to the level of the fundus (Fig. 2C). It is important to remove all bone covering the common canalicular opening. A metallic lacrimal probe is passed through inferior canaliculi and gently pushed medially to tent the lumen of the sac and to facilitate the incision on the sac. A horizontal incision then is made with a no. 12 blade on the inferior border of the exposed sac wall. After identifying the lumen, a vertical incision is made with a slit knife and extended to the fundus of the sac. An anteriorly based lacrimal sac flap is created, everted and adjusted to accurately oppose the nasal mucosa (Fig. 2D).
If a silicone bicanalicular tube is intended, it is then positioned (Fig. 2E). A small gel foam patch soaked in an antiadhesive agent is packed lightly in the exposed sac to keep the flap in position throughout the initial healing period. Light nasal packing is required unless there has been associated nasal surgery. Each patient is postoperatively prescribed oral antibiotics, nasal steroid spray and ophthalmic drops, and is followed regularly for nasal dressing. Nasal irrigation with saline is performed to prevent crust formation. The silicone tube is removed after one month.
RESULTS
Patients' ages ranged from 31 to 76 yr, with a mean age of 58.1 yr. Among the 48 patients, 12 patients had bilateral disease, 17 patients had a right-sided obstruction, and 19 patients had a left-sided obstruction.
The follow-up period ranged from 3 to 7 months, with an average of 5.2 months. Six patients (9.8%) underwent endoscopic sinus surgery in conjunction with endoscopic DCR to treat chronic rhinosinusitis and five patients (8.2%) required septoplasty during the endoscopic DCR procedure.
The levels of obstruction were the common canaliculus in 14 eyes (23.3%), the lacrimal sac in 13 eyes (21.7%), the duct-sac junction in 13 eyes (21.7%) and the nasolacrimal duct (NLD) in 20 eyes (33.3%) (Table 1). Categorized by obstruction level, ductsac junction obstruction was treated most successfully (100%), followed by NLD obstruction (90%), common canaliculus obstruction (78.6%) and saccal obstruction (69.2%) (Fig. 3). However, there was no statistically significant difference between the groups (P=0.32) (Fisher's exact test).
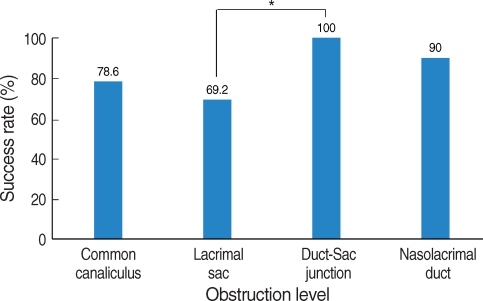
Surgical outcome of endoscopic dacryocystorhinostomy according to the obstruction levels of lacrimal drainage system. It shows that the success rate is highest in duct-sac junction obstruction (100%) and lowest in saccal obstruction (69.2%), but there is no statistically significant difference between the groups (P=0.32) (Fisher's exact test).
There were no serious complications beyond the obstruction of the neo-ostium which caused surgical failure. The surgical failure group included nine patients (3 cases of common canaliculus obstruction, 4 cases of saccal obstruction, and 2 cases of NLD obstruction) who had invisible or obstructed neo-ostium by granulation tissue or scar band. Revision procedures were recommended but were lost to follow-up.
DISCUSSION
Endoscopic DCR is an accepted technique for the management of lacrimal drainage system obstruction (4-6, 11). A satisfactory procedure is defined as freedom from epiphora at three months after surgery (8) and a healed patent neo-ostium with a free flow of tears from conjunctiva to the nose.
Many factors influence the outcome of endoscopic DCR. One of the most important prognostic factors is the obstruction level in the lacrimal drainage system. However, it is not easy to compare published success rates of lacrimal surgery because different studies use different methods to determine the obstruction level and use different criteria of successful outcomes. There are many clinical tests for the evaluation of the lacrimal drainage system. Canalicular probing and Jones' test are reliable in identifying puntal obstruction and canalicular obstruction, but they are not reliable in determining the exact level of an obstruction beyond the common canaliculus. The stenosis of sac or duct can be identifiable with DCG and it is an accepted standard method to localize the obstruction level.
This study showed that the most common level of obstruction was the nasolacrimal duct (33.3%), followed by common canaliculus (23.3%), lacrimal sac (21.7%), and duct-sac junction (21.7%), which is similar to previous reports (12).
Yung and Haedman-Lea (8) reported the results of endoscopic primary DCR in 171 watering eyes after 6 months and found the highest success rates in patients with lacrimal duct-sac obstruction (93% of cases) and with common canalicular blockage (88% of cases). Grover et al. (13) reported the operation to be 68% successful in patients with obstruction of common canaliculus using the modified canaliculo-DCR technique. Our results were similar. We also found duct-sac junction obstruction and NLD obstruction showed good surgical outcomes (100% and 90% respectively) and that common canaliculus obstruction was more difficult cure (78.6% success rate). However, we classified obstruction levels more strictly and we focused on saccal obstruction. Though there was no statistically significant difference between groups, the newly classified group (saccal obstruction) showed a relatively lower success rate (69.2%). A key factor of success in endoscopic DCR is to expose the sac fully and to make a wide neo-ostium. However, it is difficult to make a wide neo-ostium in patients with saccal obstructions because of granulation tissue formation, fibrosis or contraction of the sac itself. Therefore, patients with lacrimal sac obstruction are expected to have a poorer prognosis and to have more difficulty during surgical procedure.
This study may help to predict the prognosis of patients with lacrimal system obstruction more exactly. Also, it is important that we found lacrimal sac obstruction as a new prognostic factor. However, this study has small sample size of patients so further study is needed with larger group of patients.
In patients with lacrimal drainage system obstruction, preoperative confirmation of obstruction level using DCG may be helpful to predict patients' prognosis after endoscopic endonasal DCR. Patients with saccal obstruction may have a poorer prognosis.
Notes
This work was supported by Chungbuk National University Grant in 2008.